All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MPN Advocates Network.
The mpn Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mpn Hub cannot guarantee the accuracy of translated content. The mpn and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The MPN Hub is an independent medical education platform, sponsored by AOP Health, GSK, Sumitomo Pharma, and supported through educational grants from Bristol Myers Squibb and Incyte. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MPN content recommended for you
Factors predisposing failure to reach allogeneic hematopoietic stem cell transplantation in patients with myelodysplastic syndromes
Myelodysplastic syndromes (MDS) are myeloid malignancies with a median survival of less than 1 year, with a third of cases possessing a higher-risk disease at diagnosis. The only curative treatment is allogeneic hematopoietic stem cell transplantation (HSCT), but the eligibility process is complex. Lindholm et al.1 studied the proportion of patients failing to reach eligibility for HSCT and the factors predisposing failure, and their results were recently published in Bone Marrow Transplantation. We summarize the study below.
Study design
The study consisted of two cohorts of patients diagnosed with either MDS or MDS/myeloproliferative neoplasms (MDS/MPN) with intent to proceed to HSCT.
Group 1
Patients were between 18 and 74 years old, and included in the Swedish MDS registry. The study group consisted of patients considered suitable for HSCT between 2009–2015. Patient characteristics are shown in Table 1.
Group 2
Consecutive patients aged between 18 and 74 years old from the Karolinska University Hospital, Stockholm, SE, were included in this cohort. All patients were diagnosed from 2000 to 2018 and treated from 2004 to 2019. Causes of failure to reach HSCT were categorized as follows:
- Progressive/refractory disease
- No suitable donor
- Infection
- Comorbidity
A total of 130 patients were included in Group 2. HSCT was performed after a median of 175 days after the documentation of the patient being an HSCT candidate, and a median of 280 days after diagnosis. Out of Group 2, 109 patients received disease-modifying therapies (azacitidine or integrative cancer therapies). Patient characteristics for this group, as well as for Group 1, are shown in Table 1.
Table 1. Patient characteristics*
|
HSCT, hematopoietic stem cell transplantation; IPSS-R, revised International Prognostic Scoring System; MDS/MPN, myelodysplastic syndromes/myeloproliferative neoplasms. |
||
|
Characteristic |
Group 1 |
Group 2 |
|---|---|---|
|
Age at diagnosis, median (range) |
58 (18–73) |
60 (18–74) |
|
Days until HSCT from diagnosis, median (range) |
— |
280 (56–5,453) |
|
Male/female, % |
58/42 |
63/37 |
|
Comorbidity index at HSCT decision, median (range) |
— |
2 (0–10) |
|
Transfusion dependent (erythrocytes), % |
50 |
47 |
|
Mixed MDS/MPN, % |
19 |
15 |
|
IPSS-R risk group, % |
||
|
Very low |
2 |
6 |
|
Low |
12 |
15 |
|
Intermediate |
18 |
33 |
|
High |
27 |
21 |
|
Very high |
41 |
25 |
|
IPSS-R prognostic subgroup (karyotype), % |
||
|
Very good |
0.5 |
2 |
|
Good |
39 |
55 |
|
Intermediate |
22 |
13 |
|
Poor |
15 |
14 |
|
Very poor |
24 |
16 |
Results
Characteristics of patients who failed to reach HSCT
A total of 25% of patients in Group 1 failed to reach eligibility for HSCT compared with 22% of patients in Group 2. In Group 2, the time between the date the patient was identified as a potential HSCT candidate and when the patient was considered ineligible for HSCT was 153 days. The reasons for failed HSCT eligibility in Group 2 are shown in Figure 1.
Figure 1. Reasons of failure to reach HSCT in Group 2*
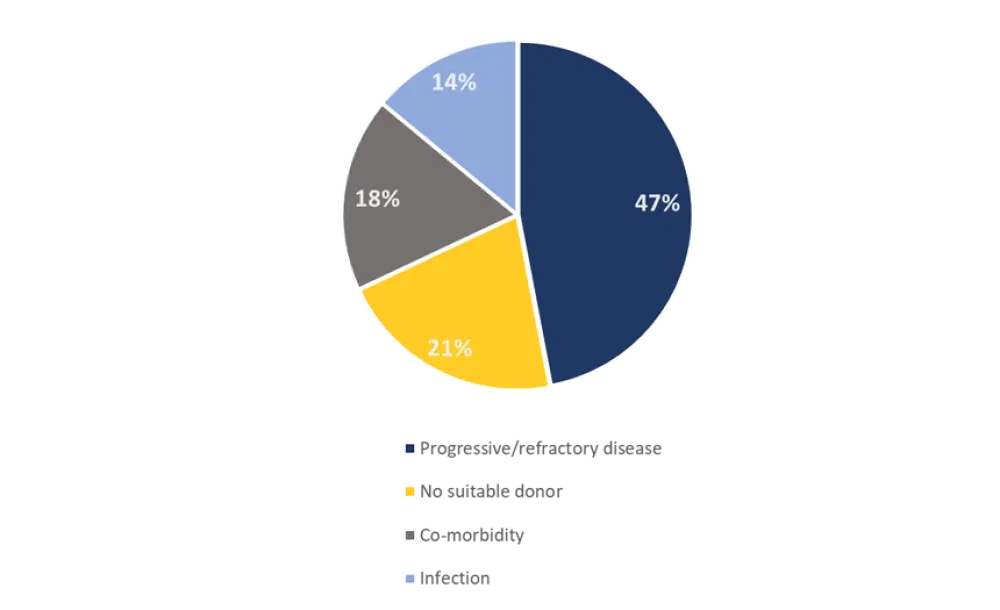
*Adapted from Lindholm et al.1
All patients who experienced progressive/refractory disease (n = 13) received cytoreductive therapy (Figure 2).
Figure 2. Proportion of patients receiving cytoreductive therapy*
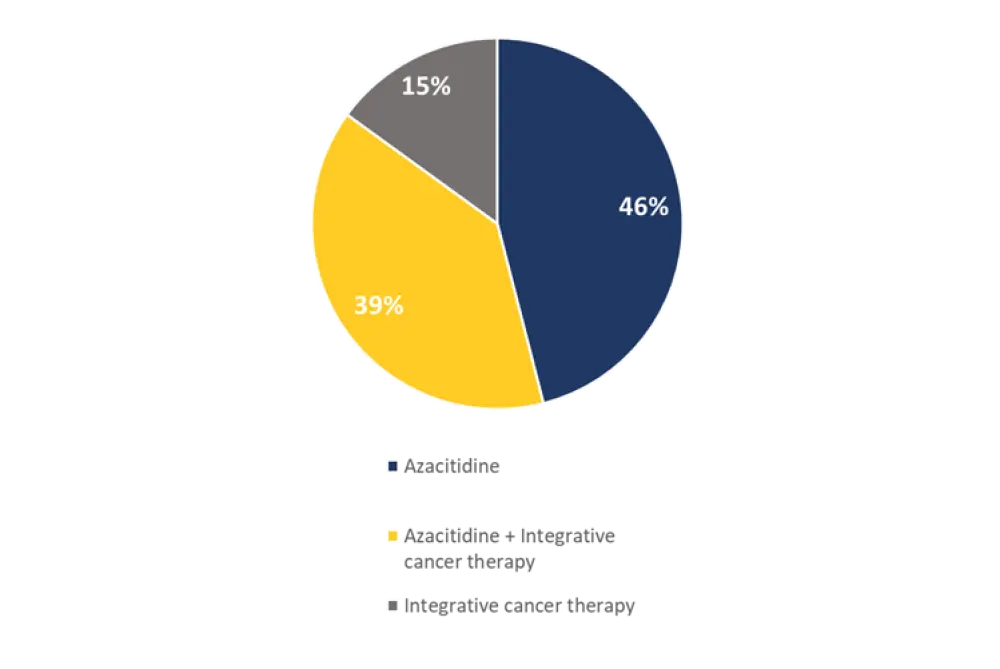
*Adapted from Lindholm et al.1
The type of comorbidity causing the cessation of treatment is shown in Figure 3. All infections identified among the patient cohort were fungal and led to the cessation of treatment.
Figure 3. Comorbidities causing cessation of treatment*
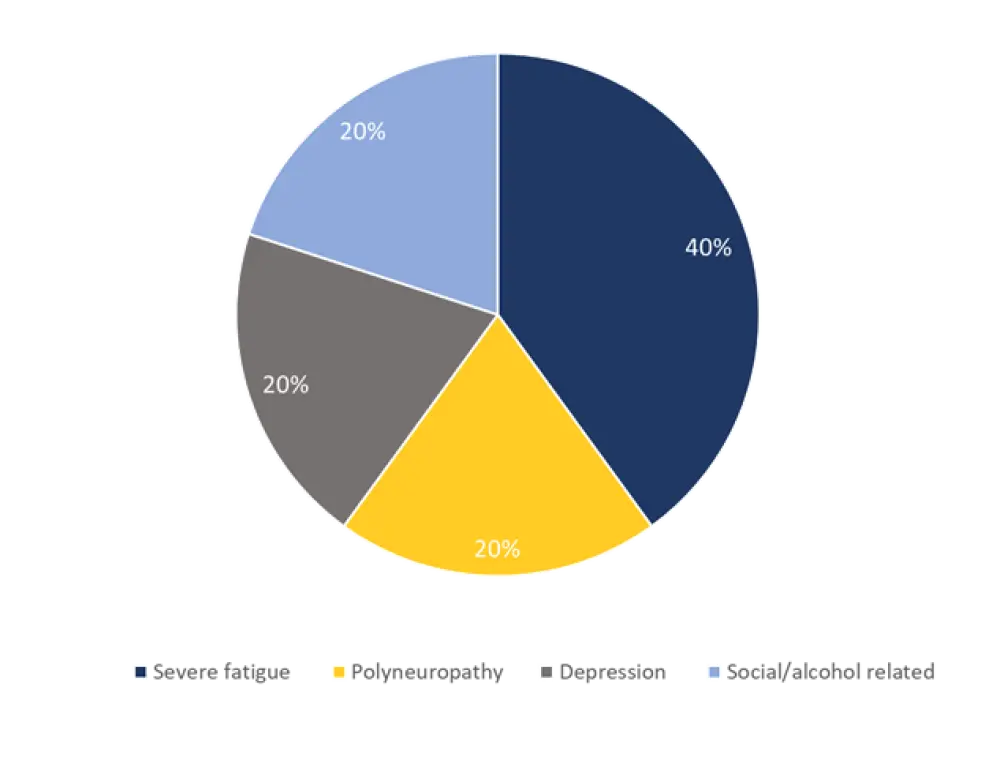
*Adapted from Lindholm et al.1
Factors associated with failure to reach HSCT
Univariate analysis of Cohort 1 identified several factors associated with a higher failure rate to reach HSCT:
- Age
- Mixed MDS/MPN, 36%
- IPSS-R low, 39%
- Lower marrow blast count, 36%
- IPSS-R karyotype – very poor, 33%
The factors associated with a higher failure rate to reach HSCT in Group 2 were: age and IPSS-R karyotype – poor (39%).
There was no significant difference in failure rate to reach HSCT between treatment with azacitidine or integrative cancer therapies; the failure rates were 22% and 28%, respectively.
Multivariate analysis of failure rate to reach HSCT, in Group 1, included all variables with p value ≤ 0.1 in the univariate analysis:
- Age at diagnosis
- Marrow blast category 0–4.9% and >0%
- Hemoglobin level category ≥10 g/dL
- WHO 2016 subgroup mixed MDS/MPN
- Therapy-related disease
- IPSS-R karyotype – very poor
- Blast count 0–4.9%
The variables included in the multivariate analysis of Group 2 are as follows:
- Age at diagnosis
- Comorbidity index
- Hemoglobin ≤7.9
- IPSS-R karyotype – intermediate and poor
The results for the multivariate analysis are shown in Table 2.
Table 2. Multivariate analysis*
|
IPSS-R, revised International Prognostic Scoring System; MDS, myelodysplastic syndromes; MPN, myeloproliferative neoplasms; WHO, World Health Organization. |
||||||
|
Variable |
Cohort 1 |
Cohort 2 |
||||
|---|---|---|---|---|---|---|
|
OR |
95% CI |
p value |
OR |
95% CI |
p value |
|
|
Age at diagnosis |
1.05 |
1.02–1.09 |
0.003 |
1.05 |
1.00–1.09 |
0.04 |
|
Therapy-related disease |
1.74 |
0.79–3.87 |
0.17 |
— |
— |
— |
|
Comorbidity index |
— |
— |
— |
1.2 |
0.98–1.53 |
0.07 |
|
Marrow blast 0–4.9% |
2.59 |
1.39–4.82 |
0.003 |
— |
— |
— |
|
Marrow blast 10.1–19.9% |
0.50 |
0.21–1.19 |
0.12 |
— |
— |
— |
|
Hemoglobin |
||||||
|
≥10 g/dL |
0.45 |
0.24–0.87 |
0.02 |
— |
— |
— |
|
≤7.9 g/dL |
— |
— |
— |
2.9 |
0.62–12.8 |
0.18 |
|
WHO 2016 mixed MDS/MPN |
1.40 |
0.56–3.39 |
0.48 |
— |
— |
— |
|
IPSS-R prognostic subgroup (karyotype) |
||||||
|
Intermediate |
— |
— |
— |
0.35 |
0.04–2.95 |
0.33 |
|
Poor |
— |
— |
— |
2.44 |
0.80–7.43 |
0.12 |
|
Very poor |
2.0 |
1.01–4.12 |
0.05 |
— |
— |
— |
Survival – Group 1
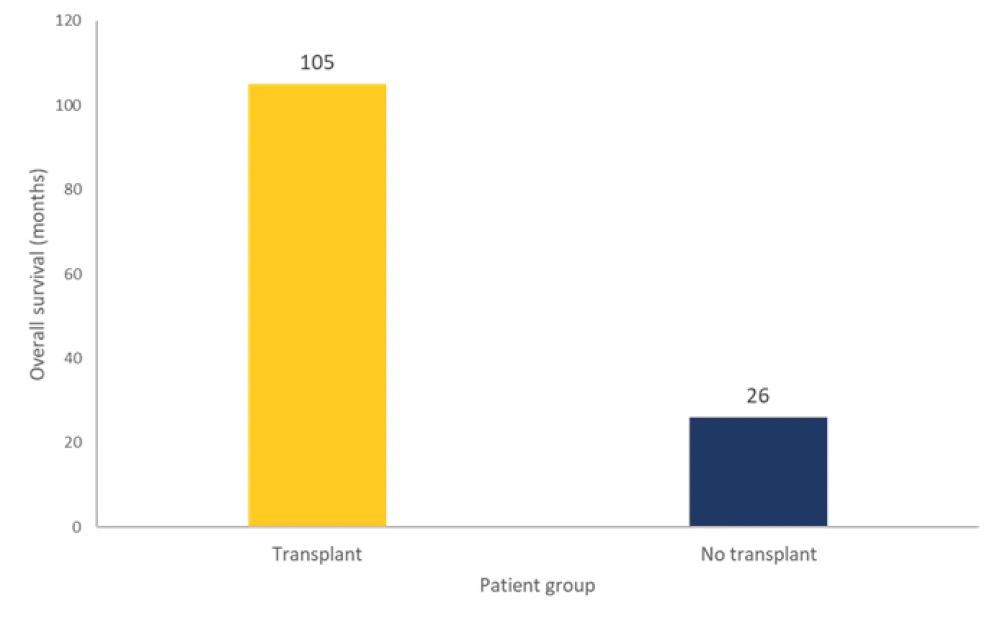
A total of 129 patients in Group 1 were still alive at data cutoff, with a median follow-up time of 29 months. The overall survival (OS) of patients receiving transplantation compared to those who received no treatment is shown in Figure 4. Transplantation also showed a significant survival benefit for all patients in the MDS/MPN group, as well as every IPSS-R group (except for low and very low).
Figure 4. OS rate for transplanted patients vs patients who failed to reach HSCT in Group 1*
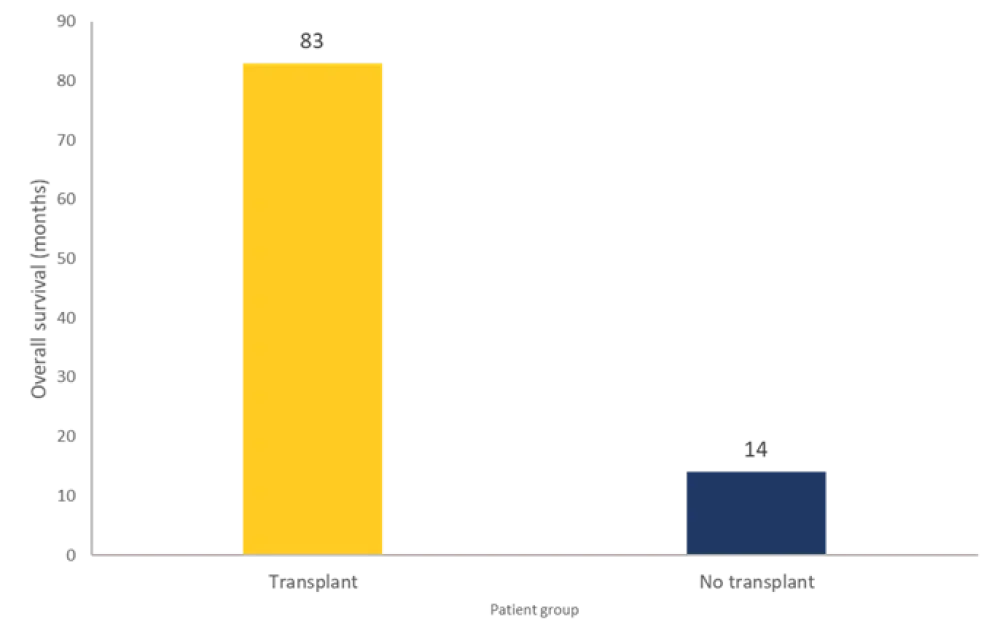
OS, overall survival; HSCT, hematopoietic stem cell transplantation.
*Adapted from Lindholm et al.1
Survival – Group 2
A total of 70 patients were still alive at data cutoff, with a median follow-up time of 41.5 months. The OS rate was 82 months. The OS of transplanted patients vs those who received no treatment is shown in Figure 5. From this group, 27 patients relapsed post-HSCT at a median of 10 months, and 18 died due to nonrelapse mortality at a median of 4 months. The 22 patients who failed to reach HSCT are now deceased. The median time from confirming unsuitability to death was 1.4 months. The causes of death were disease progression (64%), infection (32%), and pulmonary embolism (4%).
Figure 5. OS rate for transplanted patients vs patients who failed to reach HSCT in Group 2*
OS, overall survival; HSCT, hematopoietic stem cell transplantation.
*Adapted from Lindholm et al.1
Conclusion
A significant proportion of patients still fail to reach HSCT and is often down to both a difficult and complex process involving patient and donor issues. The most frequent cause of failure found was progressive/refractory disease and highlights the importance of disease surveillance, active treatments, and novel induction/conditioning approaches to bridge therapeutic options and increase the chances of patients reaching transplantation.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

