All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MPN Advocates Network.
The mpn Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mpn Hub cannot guarantee the accuracy of translated content. The mpn and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The MPN Hub is an independent medical education platform, sponsored by AOP Health, GSK, Sumitomo Pharma, and supported through educational grants from Bristol Myers Squibb and Incyte. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MPN content recommended for you
Patient reliance on social media for health information
Rare diseases may require special attention when it comes to effective communication among healthcare stakeholders. The use of the Internet is on the rise among patients to access information outside of clinical settings. Increased use of social media platforms has made it easier for patients with rare diseases to increase their understanding of the disease and to connect with the community. Healthcare professionals now are more active on social media, particularly on Twitter, to disseminate accessible information and to facilitate discussions related to their fields.
Nevertheless, the level of disease-specific knowledge among patients with myeloproliferative neoplasms (MPN) and to what extent these patients use social media or online resources to seek information is unclear. Better understanding of these patient behaviors may indicate a need to improve access to accurate resources. Pemmaraju et al. conducted a study to evaluate disease knowledge and awareness amongst patients with MPN and recently published their results in Leukemia & Lymphoma.1
Study design
- The study population was composed of patients who participated in the Patient Power online community and who self-identified with an MPN diagnosis as a patient or caregiver (N = 4,314).
- A 38-item online questionnaire was developed and distributed online among the participants.
- Questions covered the following main points:
- Type of MPN.
- Awareness about genetic/molecular markers.
- Awareness about presence of any molecular markers in addition to JAK2, CALR, MPL, or triple negative.
- Level of disease risk described by the physician at the time of diagnosis.
- Awareness about karyotype, such as diploid, +8, -7/7q-, I[17q], -5/5q-, 12p-, inv[3], or 11q23.
Results
A total of 983 patients completed the questionnaire. The most frequently reported symptom in participants was fatigue, followed by headache, abdominal pain, pruritis, and night sweats. Also, 13% reported to have one or more family member with MPN, and 25% stated to have other blood cancer diagnosed in their family members. Important patient characteristics are included in Table 1.
Table 1. Patient demographics*
|
*Adapted from Pemmaraju N et al.1 |
||
|
Characteristic |
Variable |
Patients |
|---|---|---|
|
Mean age, years (range) |
59.9 (20–90) |
|
|
Age at diagnosis, % |
21–30 |
5 |
|
31–40 |
12 |
|
|
41–50 |
21 |
|
|
51–60 |
29 |
|
|
61–70 |
26 |
|
|
71–80 |
6 |
|
|
80+ |
1 |
|
|
Gender, % |
Female |
74 |
|
Level of education, % |
High school diploma or equivalent |
10 |
|
College credit, no degree |
18 |
|
|
Bachelor’s degree |
25 |
|
|
Master’s degree |
20 |
|
|
Ethnicity, % |
Caucasian |
93 |
|
Major location for treatment, % |
Cancer center |
52 |
|
Doctor's office |
29 |
|
|
Types of diagnosis, % |
Polycythemia vera |
41 |
|
Essential thrombocythemia |
33 |
|
|
Myelofibrosis |
22 |
|
|
Risk level described by physician, % |
High |
21 |
|
Intermediate |
20 |
|
|
Low |
26 |
|
|
Not described/unsure |
33 |
|
|
Comorbidities, % |
Hypertension |
30 |
|
Venous thromboembolism |
20 |
|
|
Previous cerebrovascular incident |
11 |
|
|
Other |
15 |
|
|
History of other malignancy, % |
Solid cancer |
15 |
|
Hematological cancer |
3 |
|
|
Event leading to diagnosis, % |
Abnormal blood test result |
74 |
|
Fatigue |
28 |
|
|
Headache |
20 |
|
|
Pruritis |
14 |
|
|
Night sweats |
14 |
|
|
Abdominal discomfort |
11 |
|
|
Lack of concentration |
10 |
|
Fatigue was reported as the most common symptom. The majority of the patients reported an improvement in symptoms with treatment, mostly on hydroxyurea, low-dose aspirin, phlebotomy, and ruxolitinib. Patient responses are included in Table 2.
Table 2. Treatment and subjective responses*
|
*Adapted from Pemmaraju et al.1 |
||
|
Variable |
Patients |
|
|---|---|---|
|
Treatment |
Anagrelide |
167/716 (23) |
|
Hydroxyurea |
636/877 (73) |
|
|
Hypomethylating agent |
16/678 (2) |
|
|
Interferon |
94/683 (14) |
|
|
Ruxolitinib |
239/742 (32) |
|
|
Low dose aspirin |
795/899 (88) |
|
|
Pegylated interferon |
157/717 (22) |
|
|
Phlebotomy |
441/788 (56) |
|
|
Stem cell transplantation |
19/671 (3) |
|
|
Corticosteroids |
56/681 (8) |
|
|
Thalidomide, lenalidomide, or other IMiD drug |
11/671 (1) |
|
|
Clinical trial therapy/ combination therapy |
67/688 (10) |
|
|
Improvement after treatment initiation |
Yes |
599/942 (64) |
|
No |
211/942 (22) |
|
|
No symptoms/no treatment received |
132/942 (14) |
|
|
Treatment leading to symptom improvement, n (%) |
Anagrelide |
26 (4) |
|
Hydroxyurea |
316 (53) |
|
|
Hypomethylating agent |
4 (1) |
|
|
Interferon |
23 (4) |
|
|
Ruxolitinib |
166 (28) |
|
|
Low dose aspirin |
193 (32) |
|
|
Pegylated interferon |
72 (12) |
|
|
Phlebotomy |
192 (32) |
|
|
Stem cell transplantation |
13 (2) |
|
|
Corticosteroids |
15(3) |
|
|
Thalidomide, lenalidomide, or other IMiD drug |
5 (1) |
|
|
Clinical trial therapy/combination therapy |
23 (4) |
|
|
Other |
50 (8) |
|
- Among 234 respondents, 6% underwent stem cell transplantation and 18% were considering it.
- 10% of patients who participated in an MPN clinical trial learnt about clinical trials from their physician, a conference, or social media.
- Most patients (89%) used Internet/online resources for information about MPN therapies prior to or in between doctor visits.
- 95% of patients were frequent users of online resources, while some used online resources either a week before (3%) or on the day of (1%) a doctor visit.
- Online support resources were used to learn about MPN or therapies (86%), see laboratory data (43%), clinical trials (28%), connect with other people with a shared condition (72%), prepare for visits and make care decisions (57%), and improve patient–provider communication (44%).
- Twitter was the preferred medium for sharing medical knowledge by physicians and investigators, while patients preferred Facebook, Google, or YouTube.
Figure 1 shows the patient responses to the question regarding which social media platforms they used to research their condition.
Figure 1. Patient use of social media*
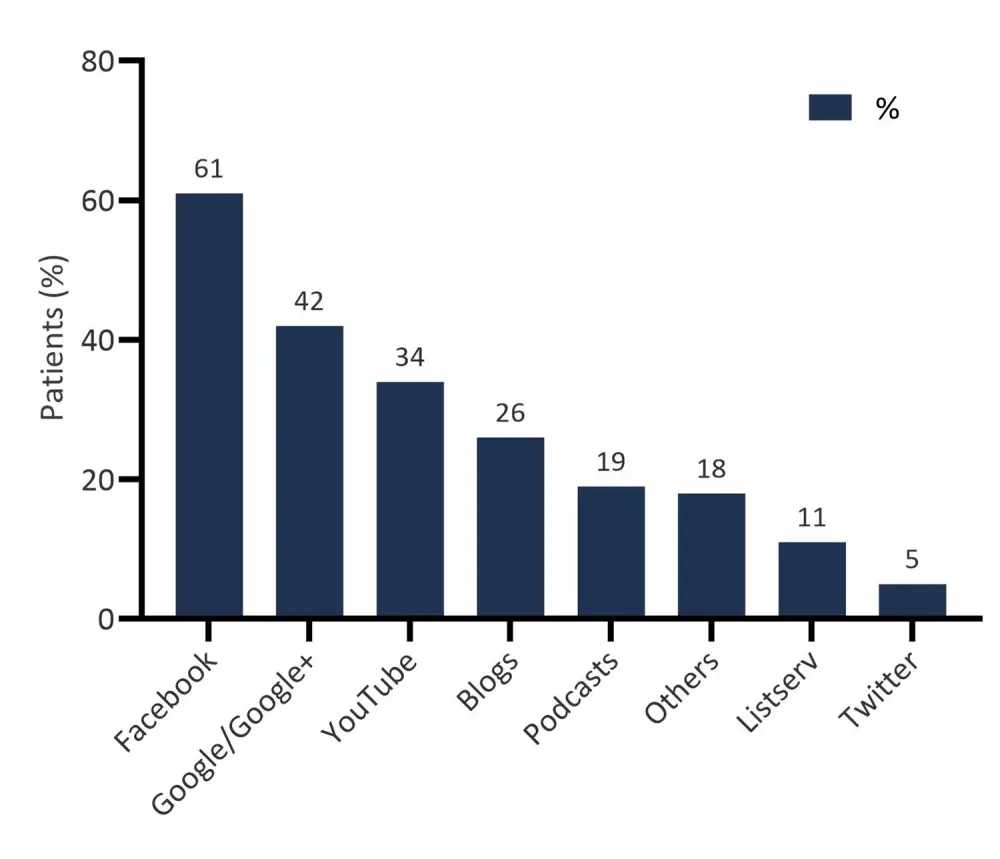
*Data from Pemmaraju et al.1
- 48% of patients were interested in patient care through online/Internet-based activity facilitated by their physician’s office.
- It was revealed that online information sharing helped the responders in several ways, including increased disease awareness, connecting with other patients with similar health conditions, access to experts and latest research, and improvement in overall quality of life.
- 93% of patients agreed to participate in a de-identified patient registry/central database for clinical research.
Conclusion
Suggestions were made to improve the patient experience and understanding of their disease, such as more online educational tools, informative materials in physician offices, and improved strategies for physicians and their patients about MPN diagnosis, staging, basic and advanced molecular mutational assessments.
There was a difference in social media habits between physicians (Twitter being the preferred medium) and patients (who preferred other platforms), indicating that educational campaigns should be designed in more personalized ways and should aim to fit a variety of online platforms to maximize patient benefit. Nevertheless, the authors conclude that social media cannot be used as a replacement for doctor recommendation, and it is suggested that most authentic advice should only be obtained through general physicians. Direct communication between patients and physicians is vital as it helps to build trust, increases patient satisfaction, influences patient understanding of their disease, and improves treatment adherence and recovery.
Limitations of this study include self-reporting nature of patient responses for analysis, exclusion of certain MPN patients who may not have access or understanding of online surveys.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

