All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MPN Advocates Network.
The mpn Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mpn Hub cannot guarantee the accuracy of translated content. The mpn and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The MPN Hub is an independent medical education platform, sponsored by AOP Health, GSK, Sumitomo Pharma, and supported through educational grants from Bristol Myers Squibb and Incyte. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MPN content recommended for you
Prevalence of pulmonary hypertension in patients with MPN and the associated risk factors
Pulmonary hypertension (PH) is a serious condition that can present with right ventricular dysfunction, fatigue, dyspnea, syncope, chest pain, palpitations, and lower extremity edema. It is defined as a mean pulmonary artery pressure (mPAP) ≥ 25 mmHg when diagnosed by right heart catheterization (RHC), or > 35 mmHg when diagnosed by trans-thoracic echocardiography (TTE). The frequency of PH has been shown to be elevated in patients with Philadelphia-chromosome negative myeloproliferative neoplasms (MPN), such as polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF), and the prognosis for these patients is fairly poor, with a median survival of ~ 2.8 years.1
Prevalence estimates of PH in patients with MPN vary between studies from < 4% to > 50%. Many confounding factors could contribute to this variance, such as the criteria for patient selection, the diagnostic tool used, MPN subtype, duration of MPN, and age. Therefore, our MPN Hub Steering Committee member, Tiziano Barbui, and colleagues carried out a systematic review and meta-analysis to estimate prevalence and predict risk factors for PH in patients with MPN. The results were recently published in the European Journal of Haematology and are summarized below. 1
Study design and characteristics1
- For the systematic review, the terms “myeloproliferative disorders”, “polycythemia vera”, “essential thrombocythemia”, “myelofibrosis”, and “pulmonary hypertension” were searched for in MEDLINE, EMBASE, and Clinicaltrials.gov, for reports between 1999–2019
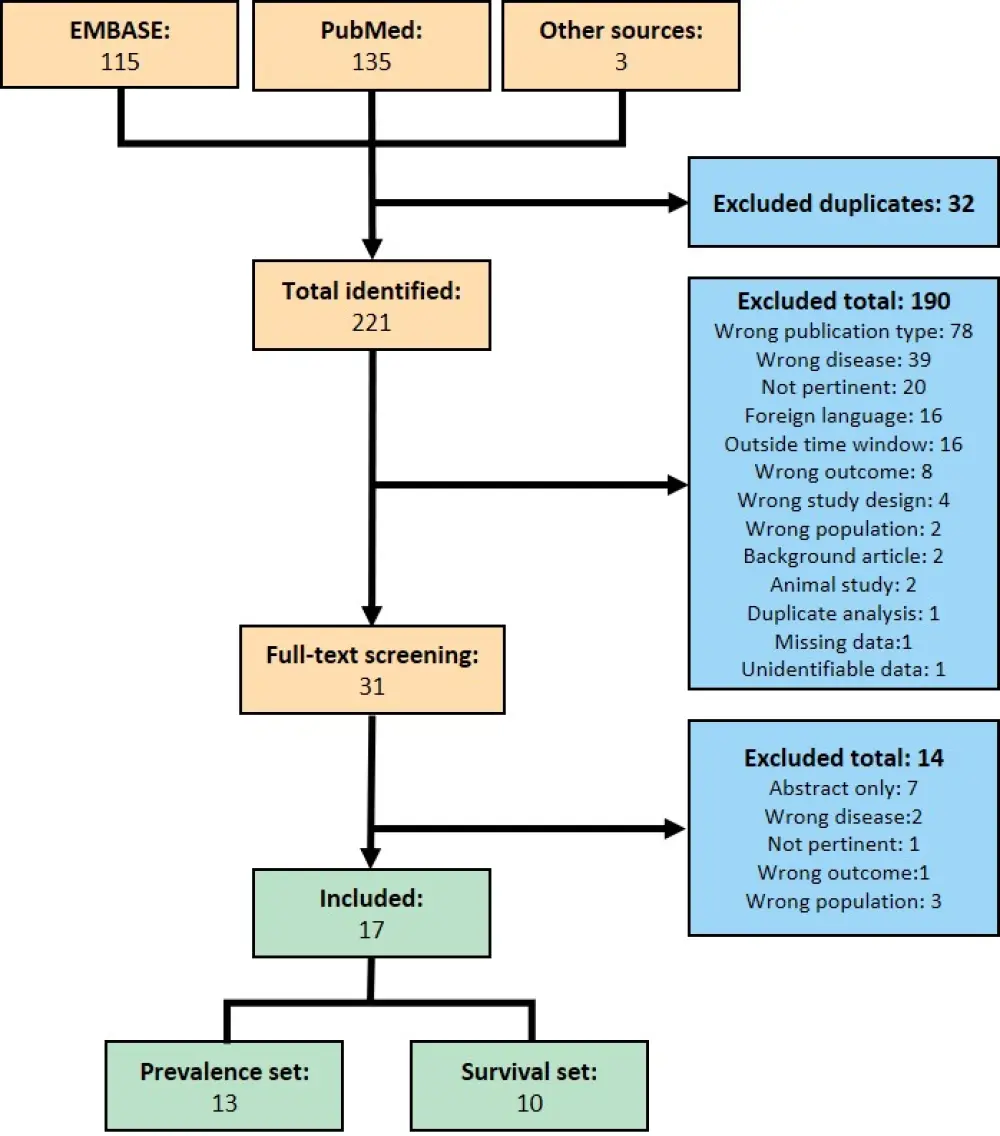
- There were 221 reports (after the removal of duplicates)
- After further screening, 17 papers remained and were included in the review (Figure 1)
Figure 1. Screening process for study inclusion1
- Study quality was evaluated by the Newcastle-Ottawa scale for non-randomized trials, appropriately modified for prevalence studies
- Data extraction: number of patients with MPN evaluated, number of patients with MPN-associated PH, study duration, MPN disease duration, diagnostic method for evaluation of PH, type of MPN, patients’ age, and overall survival
- Prevalence of PH was obtained by pooling events and patient counts over studies and re-calculated by a mixed effect logistic regression model to account for study heterogeneity
- Risk factors were evaluated by a second mixed effect logistic regression model
- Study characteristics can be seen in Table 1
Table 1. Characteristics of included studies1
|
PH, pulmonary hypertension; RHC, right heart catheterization; TTE, trans-thoracic electrocardiogram; unspec, unspecified. |
|||||||
|
Publication |
Study type |
Diagnosis method |
N |
n, PH |
Prevalence of PH, % |
Median age at diagnosis of PH |
Median disease duration, years |
|---|---|---|---|---|---|---|---|
|
Garcia-Manero et al. 1999 |
Case series |
TTE |
6 |
6 |
– |
58.2 |
5.2 |
|
Dingli et al. 2001 |
Retrospective (Descriptive) |
RHC/ unspec. |
25 |
25 |
– |
74.0 |
8.0 |
|
Guilpain et al. 2008 |
Case series |
RHC/ unspec. |
10 |
10 |
– |
– |
13.5 |
|
Tabarroki et al. 2014 |
Prospective cohort |
TTE |
15 |
155 |
– |
– |
5.6 |
|
Kadikoylu et al. 2004 |
Prospective cohort |
TTE |
28 |
4 |
14.3 |
67.3 |
3.1 |
|
Gupta et al. 2006 |
Prospective cohort |
TTE |
23 |
12 |
52.2 |
54.5 |
6.0 |
|
Altintas et al. 2007 |
Prospective cohort |
TTE |
46 |
22 |
47.8 |
45.0 |
2.9 |
|
Cortelezzi et al. 2008 |
Case control |
TTE |
36 |
13 |
36.1 |
– |
3.3 |
|
Burgstaller et al. 2013 |
Case series |
RHC/ unspec. |
22 |
1 |
4.5 |
– |
– |
|
Mattar et al. 2016 |
Retrospective cohort |
TTE |
60 |
7 |
11.7 |
– |
– |
|
Austin et al. 2019 |
Retrospective cohort |
TTE |
25 |
14 |
56.0 |
70.5 |
2.5 |
|
Garypidou et al. 2004 |
Retrospective cohort |
TTE |
22 |
9 |
40.9 |
63.8 |
4.7 |
|
Chebrek et al. 2014 |
Retrospective cohort |
TTE |
71 |
3 |
4.2 |
80.0 |
1.3 |
|
Kim et al. 2019 |
Retrospective cohort |
TTE |
180 |
105 |
58.3 |
71.9 |
6.6 |
|
Brabrand et al. 2019 |
Retrospective cohort |
RHC/ unspec. |
158 |
6 |
3.8 |
70.5 |
4.0 |
|
Gupta et al. 2019 |
Retrospective cohort |
TTE |
65 |
37 |
56.9 |
65.0 |
2.3 |
|
Lopez-Mattei et al. 2020 |
Retrospective cohort |
TTE |
143 |
20 |
14.0 |
73.5 |
3.6 |
Results1
- Quality of the studies was low based on the Newcastle-Ottawa scale, as only three studies scored ≥ 4 points
- Most studies were published before the establishment of new standards for MPN diagnosis in 2008
- Sample sizes were small: only six studies had N > 50 patients with MPN
Prevalence
- Overall prevalence of pulmonary hypertension across all studies was 28.8%, however the inter-study heterogeneity was extremely high (Intraclass Correlation Coefficient [ICC] 0.33)
- Over half of the heterogeneity was attributed to the following factors: method of diagnosis, median age, percentage of patients with myelofibrosis (MF) in the sample, and disease duration. Accounting for these factors reduced the ICC to 0.15
- A mixed effect logistic regression model that included a random study effect and fixed effects for these factors showed significant impact for:
- Method of diagnosis (RHC odds ratio [OR], 0.12; 95% CI, 0.02–0.56), with a predicted mean prevalence by TTE and RHC of 34% and 7.2%, respectively
- Percentage of patients with MF (OR, 1.02; 95% CI, 1.00–1.03)
- Duration of disease before onset of PH (OR, 1.68; 95% CI, 1.14–2.49)
Risk factors
- MF was the most common diagnosis and accounted for 46.7% of the total across all studies
- Comparisons of each MPN subtype showed that patients with MF had the highest prevalence of PH
- In patients with PH, most had MF (51.8%), followed by ET (24.3%) and PV (17%)
- When analyzing MF subtypes, PH was reported more frequently in patients with PMF (52%) than those with secondary MF (40%)
- Running a series of planned contrasts against the grand mean showed an increased risk of PH in patients with PMF (p = 0.004), and lower risk for patients with PV (p = 0.003)
- A regression model using PH as an outcome and median age, MPN diagnosis, diagnostic method, and duration of MPN as predictors showed:
- Prevalence of PH among patients diagnosed by RHC was far lower (OR, 0.1; 95% CI, 0.01–0.9; TTE as baseline)
- A diagnosis of MF increased the likelihood of PH (OR, 2.6; 95% CI, 1.36–4.8; PV as baseline)
- Compared to baseline risk set by patients with PV, both PMF (OR, 4.7; 95% CI, 1.9–11.1) and secondary MF (OR, 3.9; 95% CI, 1.4–10.9) had a highly significant effect on the likelihood of developing PH
Conclusion
The prevalence of PH among patients with MPN varies considerably between published studies. Factors that influence this heterogeneity were found to be the method of diagnosis of PH, median patient age, the proportion of patients with MF, and duration of disease. The risk of PH was demonstrated to be highest for patients with MF, particularly those with PMF, and lowest in patients with PV, suggesting there are important biological differences between these types of MPN.
Limitations of this study include the small cohort size of the included studies, and that the only study that prospectively defined criteria for RHC also had the lowest prevalence of PH, so could be largely responsible for the variance observed between the PH prevalence and diagnostic modalities.
To better understand the prevalence of PH in patients with MPN and its impact on morbidity and survival, future prospective trials are required and should include cross-sectional data sets representative of patients of different ages, MPN diagnoses, and duration of MPN. They should also include patient reported symptoms, objective cardiovascular function assessments, and a hierarchical diagnostic algorithm that prospectively defines which patients should undergo non-invasive and/or invasive testing to evaluate PH and its pathophysiology.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

