All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MPN Advocates Network.
The mpn Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mpn Hub cannot guarantee the accuracy of translated content. The mpn and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The MPN Hub is an independent medical education platform, sponsored by AOP Health, GSK, Sumitomo Pharma, and supported through educational grants from Bristol Myers Squibb and Incyte. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MPN content recommended for you
QoL in MPN: physical, psychological, and social impacts
During the course of disease and subsequent treatment many patients with myeloproliferative neoplasms (MPN) report impacts on their quality of life (QoL). Previous studies have identified these impacts; however, there has been no comprehensive investigation in specific areas of patients’ life. Here, we summarize results from a survey investigating the physical, psychological, and social impacts of MPN by Eppingbroek et al.1 published in Psycho-oncology.
Study design1
Patients with MPN were assessed for:
- MPN symptoms, using the MPN Symptom Assessment Form total symptom score (Figure 1);
- QoL, using the European Organization for the Research and Treatment of Cancer Quality of Life Questionnaire; and
- Disease-related factors, from a questionnaire on diagnosis, disease status, treatment(s), adverse events, and comorbidities.
Figure 1. Hierarchical MPN patient QoL assessment model*
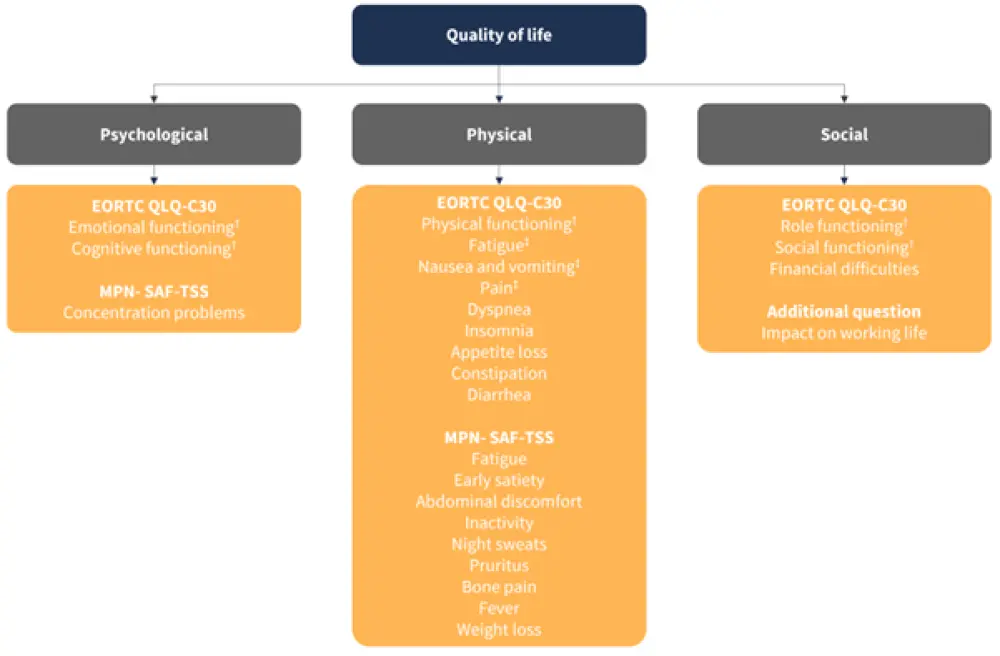
*Adapted from Eppingbroek AAM, et al.1
†Functional scales.
‡Symptom scales.
Key findings1
- Overall, 455 patients with MPN who had not received allo-SCT were recruited
- Patients were invited to answer an online survey between November 2022 and February 2023
- The mean age was 63.01 years
- 63.7% of patients were female
- 45.7% of patients were diagnosed with polycythemia vera, 17.1% with myelofibrosis, and 37.2% with essential thrombocytopenia
- Treatment options included ‘wait-and-see', phlebotomy, cytoreduction, and combined phlebotomy, and cytoreduction
Symptom burden and QoL1
- Overall, 97.4% of patients reported symptoms.
- European Organization for the Research and Treatment of Cancer Quality of Life Questionnaire scores for the most highly scored impacts in each category are outlined in Table 1.
Table 1. EORTC QLQ-C30 assessment scores for MPN patients*
|
EORTC QLQ-C30, European Organization for the Research and Treatment of Cancer Quality of Life Questionnaire; MPN, myeloproliferative neoplasms. |
||
|
Category |
QoL impact |
EORTC QLQ-C30 score |
|---|---|---|
|
Physical |
Fatigue |
44.3 |
|
|
Insomnia |
36.0 |
|
Psychological |
Cognitive function |
77.1 |
|
|
Emotional function |
66.6 |
|
|
Concentration |
74.7 |
|
Social |
Social and role function |
70.9 |
- In comparison with other cancers, patients with MPN reported fewer financial difficulties (9.9 vs 16.3) and appetite loss symptoms (10.8 vs 21.1); 48.8% of patients reported that MPN symptoms impacted on their work life.
- An increased number of reported adverse events correlated with a decrease in QoL.
- The group of patients who reported symptoms impacting working life had higher symptom burden and lower QoL compared with patients who did not (58.1 vs 69.8).
- MPN subtype and treatment option did not significantly change MPN symptom burden on QoL.
|
Key learnings |
|---|
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

