All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MPN Advocates Network.
The mpn Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mpn Hub cannot guarantee the accuracy of translated content. The mpn and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The MPN Hub is an independent medical education platform, sponsored by AOP Health, GSK, Sumitomo Pharma, and supported through educational grants from Bristol Myers Squibb and Incyte. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MPN content recommended for you
Risk of secondary malignancies in patients with MPN
Myeloproliferative neoplasms (MPN) are a group of hematological malignancies characterized by clonal proliferation of bone marrow stem cells and are classified into subgroups, including polycythemia vera, essential thrombocythemia (ET), primary myelofibrosis, chronic myeloid leukemia, and MPN unclassifiable. While the risk of developing acute myeloid leukemia is well known in patients with MPN, over the past 10 years, various studies have also reported on the increased risk of other cancers. Mette Brabrand and Henrik Frederiksen recently published a qualitative review, including 12 of these studies, which was published in the journal Cancers and is summarized below.
Study design1
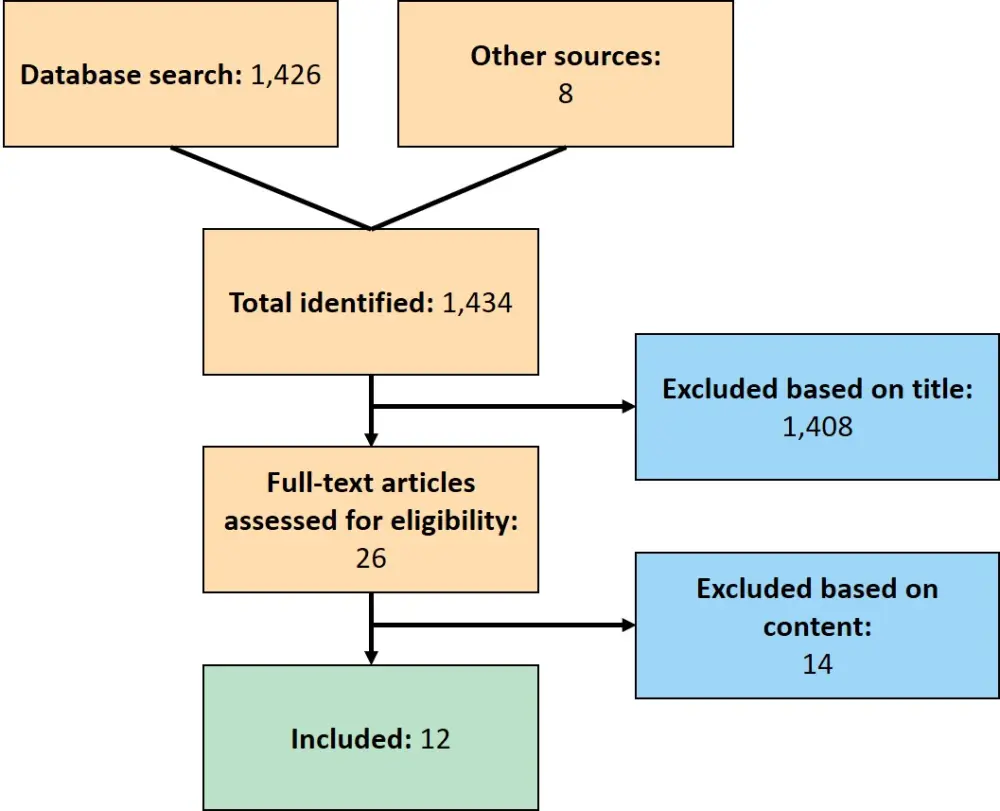
- A literature search on April 23, 2020, with the search term: “myeloproliferative neoplasm AND new primary cancer OR second cancer”, for articles published after January 1, 2000, generated 1,426 hits.
- Eight articles were identified through other sources.
- A screening process (Figure 1) yielded a retrospective cohort of 12 studies reporting on cancer occurrence after an MPN diagnosis compared to sex/age matched general population controls or to cancer incidence statistics from general population registries, which were included in the review.
- The analysis included > 65,000 patients.
- Risk estimates were abstracted from the studies, including standardized incidence ratio (SIR), incidence rate ratio (IRR), or hazard ratio (HR) between patients with MPN and the general population or another comparison group.
Figure 1. Screening and eligibility of articles for inclusion1
Results1
- The risk of new cancers was elevated 1.5–3.0-fold for patients with MPN compared with the general population.
- The incidence of solid cancers was mostly reported as SIRs/IRRs and correspond to a 1.2–1.4-fold increase (Table 1).
- The studies differed on their results of the relative estimate of cancer risk during follow-up.
- One study (Frederiksen 2011) showed that during the first 5 years following diagnosis, SIRs for cancer incidence diminished for patients with ET but increased for patients with polycythemia vera and chronic myeloid leukemia.
- Another study (Shrestha 2016) showed insignificant increases in SIR for solid cancer 2-years after diagnosis for patients with ET.
- One study (Landtblom 2018) showed HRs for any solid cancer and for non-melanoma skin cancer decreased steeply during the first year and gradually increased thereafter, though this may be reflective of coincidental findings from routine diagnostic tests during the initial MPN diagnosis process.
- The most common types of secondary solid cancers included skin, lung, thyroid, and kidney cancer (Table 1).
- Breast, prostate, and colorectal cancer occurred as frequently in patients with MPN as in the general population.
- The risk of lymphoid hematological malignancy was elevated 2.5–3.5-fold in patients with MPN compared with the general population (Table 1).
- Across all studies, patients aged 60–79 years had the largest difference in second cancer risk (1.8–4.2-fold increase) between patients with MPN and the general population.
Table 1. SIR and IRR ranges for secondary malignancies in patients with MPN1
|
CLL, chronic lymphocytic leukemia; HL, Hodgkin lymphoma; IRR, incidence rate ratio; MM, multiple myeloma; NA, not available; NHL, non-Hodgkin lymphoma; NMSC, non-melanoma skin cancer; MPN, myeloproliferative neoplasms; SIR, standardized incidence ratio. |
||||
|
Type of solid cancer |
SIR range |
Publication no(s). |
IRR range |
Publication no(s). |
|---|---|---|---|---|
|
All solid cancer |
0.8–5.2 |
3, 5, 6, 8, 10 |
1.4–1.6 |
7 |
|
Colon cancer |
0.6–1.6 |
3, 4, 5, 6, 8, 9, 10 |
0.9–1.0 |
7, 11 |
|
Lung cancer |
0.9–1.9 |
3, 4, 5, 6, 8, 9, 10 |
1.4–1.6 |
7, 11 |
|
Breast cancer |
0.8–1.3 |
3, 4, 5, 6, 8, 9, 10 |
1.0–1.1 |
7, 11 |
|
Melanoma |
1.7–3.7 |
3, 4, 5, 6, 9, 10 |
1.8–2.2 |
7, 11 |
|
NMSC |
1.0–3.3 |
3, 4, 5, 10 |
2.0 |
11 |
|
Kidney cancer |
1.1–2.4 |
3, 4, 5, 6, 8, 10 |
2.0–2.1 |
7, 11 |
|
Prostate cancer |
0.7–1.3 |
3, 4, 5, 6, 8, 9, 10 |
0.6–1.1 |
7, 11 |
|
Thyroid cancer |
0.5–3.7 |
4, 6, 9 |
2.3 |
7 |
|
Type of hematological cancer |
SIR range |
Publication no(s). |
IRR range |
Publication no(s). |
|
All NHL |
1.1–9.7 |
1, 3, 4, 6, 9 |
1.6–2.3 |
7, 11 |
|
CLL |
12.4 |
1 |
2.5 |
7 |
|
MM |
1.6 |
4 |
1.6 |
7, 11 |
|
HL |
NA |
— |
2.8–3.1 |
7, 11 |
Conclusions
Patients with MPN have an increased risk of developing secondary cancers of the skin, lung, kidney, and thyroid, as well as lymphoid cancers. This may partly be due to the treatment that patients receive, as hydroxyurea has been shown to increase the risk of non-melanoma skin cancers. Additionally, low-dose aspirin, which is used to prevent thrombosis in patients with MPN, is associated with a decreased risk of colorectal cancer, possibly because of an increased risk of gastrointestinal bleeding and therefore detection and removal of colorectal polyps.
The elevated risk of lung cancer in patients with MPN may be biased as blood test results of smokers and patients with lung disease can resemble those of patients with untreated MPN, such as high hematocrit, thrombocytosis, and leukocytosis. Therefore, these patients could be mistakenly registered with an MPN diagnosis. Nevertheless, smoking has been shown to be associated with an increased risk of developing MPN.
Age is another factor that modifies the cancer risk uniformly across studies, with the largest elevated risk increase seen for patients between 60 and 79 years. Detection bias, due to routine surveillance of patients with MPN may have influenced these results to some degree. However, as the incidence of major cancer types, such as colorectal cancer, breast cancer, and prostate cancer, were not increased among patients with MPN, detection bias is unlikely to explain the observed increased risks in specific cancer types, such as lymphoid malignancies. Although cancer surveillance among all patients with MPN may be unnecessary, it may be beneficial for those at increased risk, such as the 60–70 age group.
Table 2. Publications comparing the incidence of SMs in patients with MPN1
|
CLL, chronic lymphocytic leukemia; CML, chronic myeloid leukemia; ET, essential thrombocythemia; HL, Hodgkin lymphoma; MF, myelofibrosis; MM, multiple myeloma; MPN, myeloproliferative neoplasms; MPN-NOS, MPN-not otherwise specified; MPN-U, MPN-unspecified; NHL, non-Hodgkin lymphoma; PMF, primary myelofibrosis; PV, polycythemia vera; SM, secondary malignancy; SMF, secondary myelofibrosis. |
|||||
|
Number |
Publication |
Patient no. |
MPN subtype |
Median years of follow-up |
Type of SM assessed |
|---|---|---|---|---|---|
|
1 |
Vannuchi, 2009 |
820 |
ET (57%), PV (43%) |
3.3 |
NHL, CLL |
|
2 |
Rumi, 2011 |
1,915 |
ET (44%), PV (34%), MF (18%), SMF (4%) |
5.2 |
— |
|
3 |
Frederiksen, 2011 |
7,229 |
ET (22%), PV (63%), CML (14%) |
ET, 4.0; PV, 5.0; CML, 2.4 |
NHL |
|
4 |
Fallah, 2011 |
3,530 |
PV |
— |
NHL, MM |
|
5 |
Susini, 2012 |
733 |
ET (51%), PV (41%), PMF (8%) |
Mean 6.5 |
— |
|
6 |
Khanal, 2015 |
3,941 |
PV |
4.7 |
NHL |
|
7 |
Brunner, 2016 |
20,250 |
ET, PV, MF, MPN-U |
3.5 |
NHL, HL, CLL, MM |
|
8 |
Shrestha, 2016 |
8,116 |
ET |
3.0 |
Lymphoma |
|
9 |
Masarova, 2016 |
417 |
ET (40%), PV (60%) |
— |
NHL |
|
10 |
Landtblom, 2018 |
9,379 |
ET (28%), PV (45%), PMF (15%), MPN-NOS (12%) |
7.7 |
Lymphoma, MM |
|
11 |
Chattopadhyay, 2018 |
13,805 |
ET (30%), PV (48%), MF (11%), MPN-NOS (12%) |
ET, 4; PV, 6; MF, 2; MPN-U. 3 |
NHL, HL, MM |
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

