All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MPN Advocates Network.
The mpn Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mpn Hub cannot guarantee the accuracy of translated content. The mpn and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The MPN Hub is an independent medical education platform, sponsored by AOP Health, GSK, Sumitomo Pharma, and supported through educational grants from Bristol Myers Squibb and Incyte. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MPN content recommended for you
Use of integrative medicine may correlate with improved symptoms and quality of life in patients with MPN
Featured:
Myeloproliferative neoplasms (MPN) are associated with a high symptom burden and the risk of progression to acute myeloid leukemia (AML). Treatment options for MPN have progressed significantly in recent years, with JAK inhibitors, for example, offering effective treatment for patients with MPN. However, from the patient perspective, the burden of disease and the need for additional symptom management strategies remains high.
Integrative medicine (IM) describes a targeted, holistic, and supportive patient-centered approach to treatment, alongside pharmacological and clinical treatments. Existing evidence indicates that cancer patients may use complementary treatments without consulting their treating physicians. There is limited evidence and a lack of awareness surrounding meaningful benefits of certain IM approaches. Here we summarize the work of Krisstina Gowin et al, published in Cancer Medicine in July 2020, describing the benefit of different IM treatments on symptom relief and quality of life (QoL) in patients with MPN.1
Study design
- International, survey-based clinical cohort study conducted in 52 countries
- Informed consent and self-report surveys were collected using an online survey platform
- Patient recruitment was performed using social media and email
- Patients were required to have English as primary language or satisfactory level of proficiency
- Only patient surveys with > 10 completed responses were included in the analysis
- The primary objective was to ascertain if IM interventions improved symptom burden relief and improved quality of life for patients with MPN
- Interventions analyzed in this survey were
-
- Nutritional advice: Mediterranean, paleo/high protein-low carbohydrates, vegetarian, plant-based, gluten-free, low-fermentable saccharides, and vegan diets
- Physical activity: Aerobic exercise, strength training, dance therapy, walking, running, golf, high-intensity training
- Mind-body practice: Yoga, tai chi, qi gong, meditation, chiropractic, osteopathy, acupuncture, progressive muscle relaxation, breath exercise, massage, mindfulness-based stress reduction support group, prayer
- Dietary supplements: Vitamin D, multivitamins, magnesium, omega 3, calcium, green tea, vitamin E, medicinal marijuana, medicinal mushrooms
- Others: Traditional Chinese medicine, Ayurveda, homeopathy
- Tools used for survey-based data collection included
-
- MPN Symptom Assessment Form Total Symptom Score (MPN-SAF TSS; symptoms)
- Patient Health Questionnaire-2 (PHQ; depression)
- Brief Fatigue Inventory Usual (BFI; fatigue)
- QoL, study specific
Patient characteristics
- Mean age was 58.2 years, with a male-to-female ratio of 1:3 and 64% of patients had been diagnosed for > 3 years
- In most patients (32%) the myelofibrosis Dynamic International Prognostic Scoring System (MF DIPSS) risk category was unknown, while 29% had Intermediate-2, 19% Intermediate-1, 12% High-, and 8% Low-risk classification
- Over 50% of patients reported no alcohol intake and 91% of patients reported themselves as non-smokers
- Using BMI criteria, 33.1% of patient were over-weight, and 17% were obese
- Common comorbidities (observed in more than 5% of patients) included degenerative joint disease, fibromyalgia, hypothyroidism, restless leg syndrome, chronic fatigue syndrome, obstructive sleep apnea, heart disease, and chronic obstructive pulmonary disease
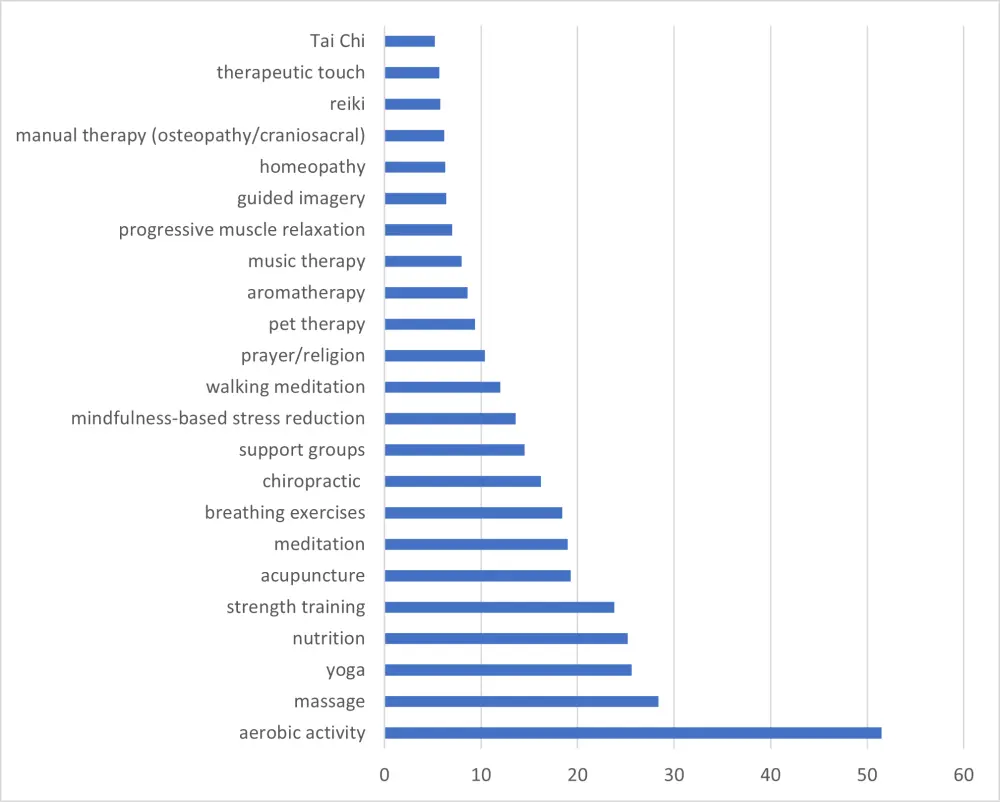
Figure 1. Integrative modalities used in > 5% of patients1
Results
Modality use
- The most commonly used integrative modalities were aerobic exercise, massage, yoga, nutrition, and strength training (for details, see Figure 1). 50.3% of patients were on active treatment for their disease while using IM modalities
- 24% of patients received nutritional advice; 10.7% of recommendations came from a hematologist, 7.5% from a registered dietician, 6.9% from a primary care physician, among other sources
- Supplementation with natural products was reported by 48.4% of patients, with 20.3% of those patients indicating they did not tell their clinician about using it
- Reasons for taking supplements included support for general health (35.8%), treating nutritional deficiencies (13.3%), managing MPN symptoms (11.5%) or non-MPN symptoms (9.8%), and influencing the course of MPN disease directly (5.0%)
- Patients considered the following support as helpful to promote the use of integrative medicine: educational resources (32.2%), insurance coverage (35%), referrals from provider (29.4%), and integrative care clinics (27.5%)
- Table 1 shows selected IM interventions with statistically significant impact (p < 0.05) on patients
Table 1. Relative scores of participants engaged in IM practices relative to those not1
|
BFI, brief fatigue inventory; MPN-SAF TSS, Myeloproliferative Neoplasm Symptom Assessment Form Total Symptom Score; QoL, quality of life. |
||||
|
Intervention/Tool |
Score of users |
Score of non-users |
P value |
Modality use vs control |
|---|---|---|---|---|
|
MPN symptom burden (MPN-SAF TSS) |
||||
|
Aerobic activity |
33.2 |
39.7 |
< 0.001 |
better |
|
Strength training |
34.0 |
37.7 |
0.013 |
better |
|
Massage therapy |
40.5 |
25.2 |
< 0.001 |
worse |
|
Support groups |
42.3 |
36.0 |
< 0.001 |
worse |
|
Omega 3 |
24.4 |
27.8 |
0.03 |
better |
|
QoL |
||||
|
Aerobic activity |
4.2 |
5.2 |
< 0.001 |
worse |
|
Strength training |
4.2 |
4.9 |
0.001 |
worse |
|
Massage therapy |
5.0 |
4.6 |
0.04 |
better |
|
Support groups |
5.4 |
4.6 |
0.002 |
better |
|
Omega 3 |
3.4 |
3.7 |
0.18 |
no difference |
|
Fatigue (BFI) |
||||
|
Aerobic activity |
5.1 |
5.9 |
< 0.001 |
better |
|
Strength training |
5.2 |
5.7 |
0.03 |
better |
|
Massage therapy |
6.1 |
5.4 |
< 0.001 |
worse |
|
Breathing techniques |
6.1 |
5.5 |
0.02 |
worse |
|
Omega 3 |
4.1 |
4.6 |
0.02 |
better |
Effect of interventions on symptoms and QoL
- Patients engaging in aerobic and strength training had better scores for symptom burden and fatigue compared to other patients, while demonstrating inferior quality of life. Conversely, patients receiving massage therapy had better quality of life, while suffering more from fatigue and symptom burden
- Supplementation with omega 3 was the only natural product which was associated with improved symptom score and fatigue
- Depression was reported in 40.7% of patients and anxiety in 46.8% of patients. Depression (PHQ score ≥ 3) was 40% less likely in patients participating in aerobic activity (OR, 0.6; 95% CI, 0.39–0.86; p = 0.006), yoga, and strength training
- 80.3% of patients reported that they did not feel their needs were heard by their healthcare provider during IM appointments
Conclusion
The study correctly identifies that symptom management, complementary treatment of the disease, and quality of life represent unmet needs of patients with MPN. IM modalities have a clear role in the management of patient symptoms but may have differential roles for the relief of specific symptoms, with an association seen for aerobic exercise and strength training and improved symptom, fatigue, and depression scores, while massage and support groups seemed to correlate with better quality of life. The role of omega 3 for symptoms and fatigue control is intriguing and may need further research. The fact that many patients reported a high degree of feeling unheard may point to a need for better training of treating physicians in IM-related aspects. Furthermore, the study identifies that only a small proportion of patients receive specific counselling and guidance in the areas studied and suggests that the universal application of IM strategies to all patients with MPN would be of benefit.
Limitations of the study include a female gender bias, the known considerations of surveys that utilize self-reporting, and the focus of the study on established and prevalent IM modalities, not those that may be accessed less frequently.
The main conclusion of the study is that further, interventional clinical research is needed to establish if IM modalities can improve the QoL and symptoms patients with MPN.
Expert Opinion
The SIMM study shows the tremendous amount of interest that exists amongst MPN patients for self driven ways to improve their quality of life, improve MPN symptoms, and perhaps impact the disease. As my co-investigators and I have found there is great enthusiasm for participating in well organized clinical trials of complementary interventions such as exercise, yoga, meditation, and nutritional interventions. We hope to evolve to bring real evidence on the benefit of these interventions and how to integrate them with evolving medical therapies.
 Ruben A. Mesa
Ruben A. MesaReferences
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

