All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MPN Advocates Network.
The mpn Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mpn Hub cannot guarantee the accuracy of translated content. The mpn and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The MPN Hub is an independent medical education platform, sponsored by AOP Health, GSK, Sumitomo Pharma, and supported through educational grants from Bristol Myers Squibb and Incyte. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MPN content recommended for you
Arterial and venous thromboembolic complication risks in patients with myeloproliferative neoplasms
Do you know... Which MPN subtype is associated with the highest risk of thromboembolic complications?
Arterial and venous thromboembolic (ATE/VTE) complications are more commonly observed in patients with myeloproliferative neoplasms (MPN) than in the general population and are associated with an increased risk of both mortality and morbidity. A study by Wille et al.1 examined the risk and incidence of ATE and VTE in patients with different MPN subtypes. The MPN Hub is pleased to summarize these findings here.
Study design1
This single-center retrospective study evaluated 832 patients with MPN for ATE/VTE complications.
ATE and VTE were shown to be associated with MPN if they occurred within two years before or following an MPN diagnosis.
Patient characteristics
At a median follow-up of 6.6 years, 180 patients experienced an ATE/VTE, with a 36.2% probability of a thromboembolic complication. The patient characteristics of the total cohort and those with a first complication are outlined in Table 1 and Table 2.
Table 1. Total cohort patient characteristics*
|
ATE, arterial thromboembolism; CALR, calreticulin; JAK2, Janus kinase 2; MPL, myeloproliferative leukemia; MPN, myeloproliferative neoplasm; VTE, venous thromboembolism. |
|
|
Characteristic, % |
Total cohort |
|---|---|
|
Male |
39.1 |
|
Female |
60.9 |
|
MPN diagnosis |
|
|
Essential thrombocytosis |
31.7 |
|
Polycythemia vera |
34.1 |
|
Myelofibrosis |
31.1 |
|
Driver mutations |
|
|
JAK2 |
69.8 |
|
CALR |
14.4 |
|
MPL |
2.5 |
|
Triple negative |
5.2 |
|
Incomplete |
8.1 |
Table 2. Patient characteristics if patients with a first complication*
|
ATE, arterial thromboembolism; MPN, myeloproliferative neoplasm; VTE, venous thromboembolism. |
|
|
Characteristic, % |
Patients with thromboembolic complications |
|---|---|
|
Time of complication |
|
|
Prior to MPN diagnosis |
32.2 |
|
At the time of MPN diagnosis |
17.2 |
|
After MPN diagnosis |
50.6 |
|
VTE |
58.3 |
|
ATE |
41.6 |
Results1
- The incidence of VTE was higher than ATE, with 58.3% vs 41.6% of patients experiencing a thromboembolic complication, respectively.
- The most common localizations of ATE were stroke, followed by transient ischemic attacks (Figure 1A).
- The most common localization of VTE was deep vein thrombosis with or without pulmonary embolism, followed by splanchnic vein thrombosis (Figure 1B).
Figure 1. Localization and incidence of A ATE and B VTE*
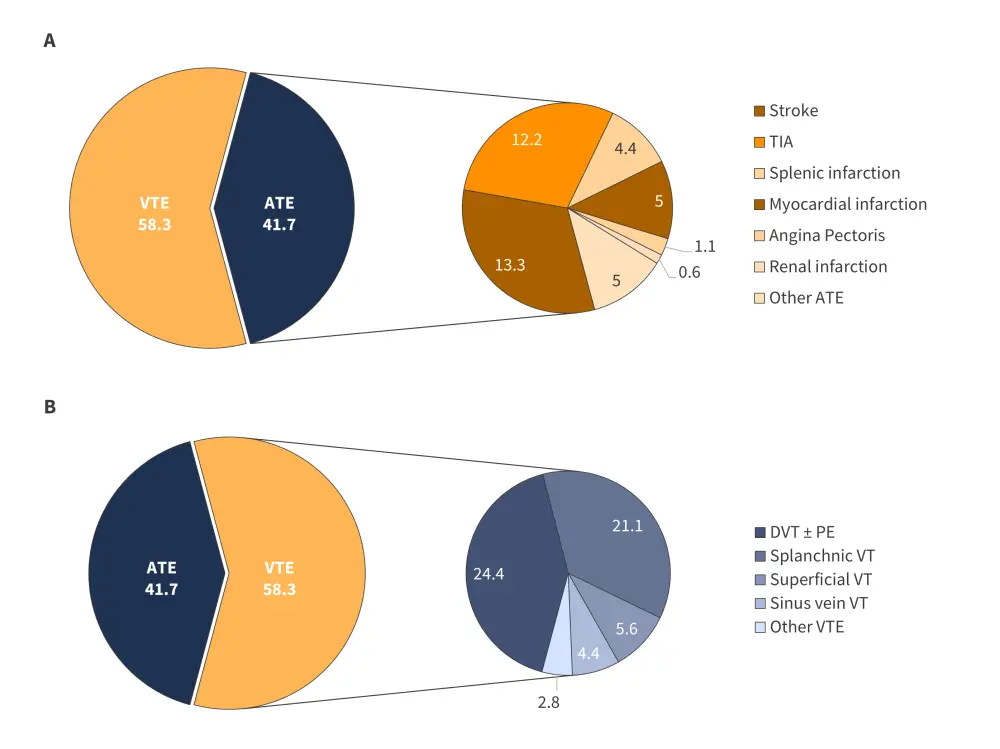
ATE, arterial thromboembolism; DVT, deep vein thrombosis; PE, pulmonary embolism; TIA, transient ischemic attack; VT, vein thrombosis; VTE, venous thromboembolism.
*Data from Wille, et al.1
The cumulative incidence of ATE and VTE was comparable in the first year of follow-up. However, VTE became more common over time; at 20 years, the incidence of ATE and VTE was 0.122 and 0.18, respectively (Figure 2).
Figure 2. Cumulative incidence for ATE and VTE over time*
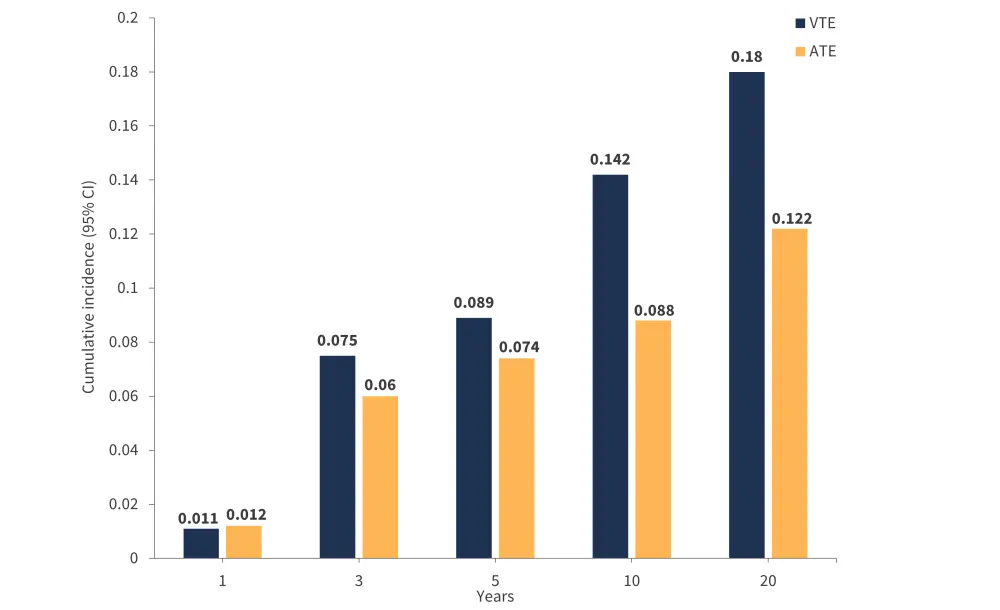
ATE, arterial thromboembolism; CI, confidence interval; VTE, vein thromboembolism.
*Data from Wille, et al.1
When comparing factors associated with an increased risk of thromboembolic complications, differences were identified in both MPN subtype and mutational status (Figure 3).
- A CALR and incomplete mutational status were associated with a significantly decreased risk compared with JAK2 mutation.
- The polycythemia vera subtype was associated with a significantly increased risk compared with other MPN subtypes.
Figure 3. Risk factors associated with an increased risk of thromboembolic complications*†‡§
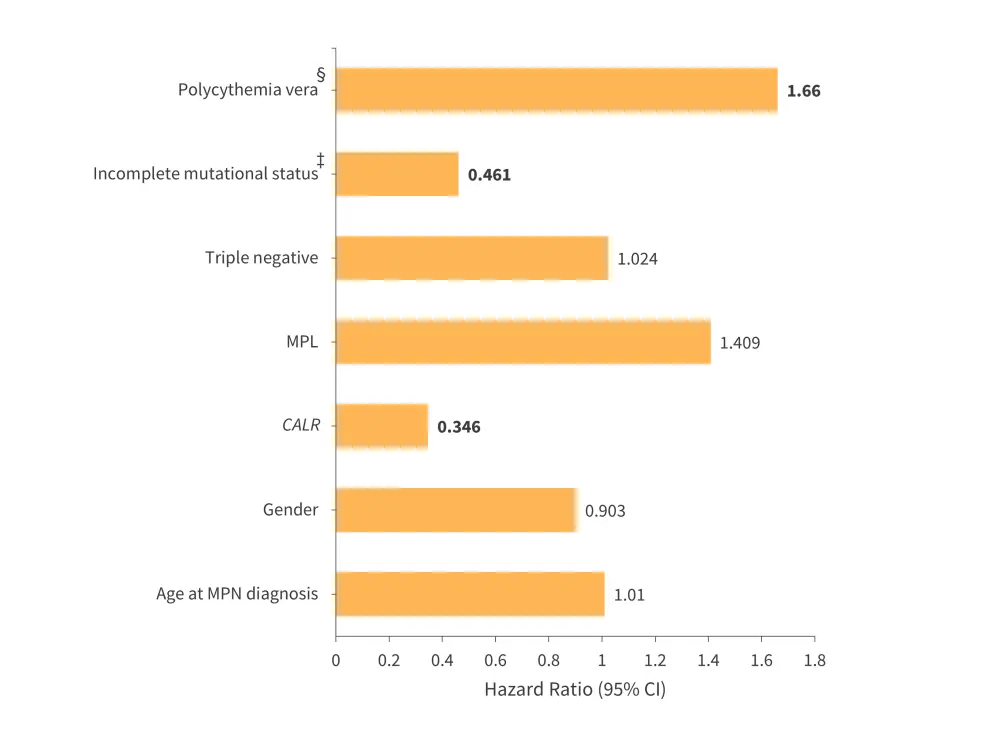
CALR, calreticulin; CI, confidence interval; MPL, myeloproliferative leukemia; MPN, myeloproliferative neoplasm.
*Data from Wille, et al.1
†Values in bold are statistically significant.
‡Mutational status are compared with JAK2 mutation.
§Polycythemia vera is compared with other MPN subtypes.
Conclusion
MPN are associated with a generally increased risk of VTE and ATE compared to a healthy population, with polycythemia vera posing the highest risk. Mutational status also influenced complications, and patients with CALR and incomplete mutational status were at a significantly decreased risk compared with other mutations, particularly the JAK2 mutated group.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

