All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MPN Advocates Network.
The mpn Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mpn Hub cannot guarantee the accuracy of translated content. The mpn and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The MPN Hub is an independent medical education platform, sponsored by AOP Health, GSK, Sumitomo Pharma, and supported through educational grants from Bristol Myers Squibb and Incyte. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MPN content recommended for you
Conditioning regimens and transplant outcomes in MF
Allogeneic hematopoietic cell transplantation (allo-HCT) is the prevailing curative treatment for myelofibrosis (MF).1 The MPN Hub has previously reported on factors influencing allo-HCT outcomes. However, optimal conditioning regimens and comparative outcomes with reduced intensity conditioning (RIC) versus myeloablative conditioning (MAC) are not well known.1
To address this knowledge gap, Murthy et al.1 recently published a study in Haematologica that evaluated the outcomes of allo-HCT for MF based on the choice of RIC or MAC conditioning regimens.1 Here we summarize key findings from the study.
Study design
- Patients aged ≥18 years with MF who underwent allo-HCT between 2008 and 2019 from the Center for International Blood and Marrow Transplant Research database were included.
- The cohort was selected based on the most common conditioning regimens used in RIC (fludarabine/busulfan vs fludarabine/melphalan) and MAC (fludarabine/busulfan vs busulfan/cyclophosphamide).
- The donor groups included:
- matched related donors;
- 8/8 (HLA-A, -B, -C, and -DRB1) matched unrelated donors; and
- 7/8 matched unrelated donors.
- The key exclusion criteria included allo-HCT from a haploidentical donor, syngeneic donor, cord blood, and ex vivo T-cell depleted or CD34 selected grafts.
Outcomes were compared separately in the RIC and MAC cohorts based on conditioning regimen, with multivariate Cox regression analysis used to evaluate factors that could influence outcomes.
The key objectives were to compare the overall survival (OS), disease-free survival, non-relapse mortality, relapse, incidence of Grade 2–3 and 3–4 acute graft-versus-host disease (GvHD), chronic GvHD, and GvHD-free relapse-free survival (GRFS) based on the choice of the conditioning regimen used with RIC or MAC.
Results
Among 872 eligible patients, 493 underwent allo-HCT using RIC (fludarabine/busulfan, n = 166; fludarabine/melphalan, n = 327) and 379 using MAC (fludarabine/busulfan, n = 247; busulfan/cyclophosphamide, n = 132). The key baseline characteristics are presented in Table 1.
Table 1. Key baseline characteristics*
|
ATG, antithymocyte globulin; Bu, busulfan; Cy, cyclophosphamide; DIPSS, dynamic international prognostic scoring system; ET, essential thrombocytosis; Flu, fludarabine; HCT, hematopoietic cell transplantation; Mel, melphalan; PV, polycythemia vera. |
||||||
|
Characteristic, % (unless otherwise stated) |
RIC |
MAC |
||||
|---|---|---|---|---|---|---|
|
Flu/Bu |
Flu/Mel |
p value |
Flu/Bu |
Bu/Cy |
p value |
|
|
Median age (range), years |
63 |
63 |
0.88 |
60 |
55 |
<0.01 |
|
Disease type |
|
|
0.22 |
|
|
0.85 |
|
Primary |
80 |
74 |
|
77 |
76 |
|
|
Post ET |
8 |
14 |
|
8 |
10 |
|
|
Post PV |
12 |
12 |
|
15 |
14 |
|
|
Median time from diagnosis to HCT (range), months |
22 |
37 |
0.02 |
25 |
38 |
0.41 |
|
DIPSS score |
|
|
0.07 |
|
|
0.03 |
|
Low/intermediate-1 |
43 |
33 |
|
54 |
61 |
|
|
Intermediate-2/high |
42 |
51 |
|
38 |
26 |
|
|
Missing |
16 |
16 |
|
8 |
14 |
|
|
Donor type |
|
|
0.75 |
|
|
0.15 |
|
HLA-identical sibling |
29 |
29 |
|
32 |
40 |
|
|
8/8-matched |
64 |
63 |
|
57 |
47 |
|
|
7/8 matched |
7 |
9 |
|
11 |
13 |
|
|
ATG/alemtuzumab use |
|
|
<0.01 |
|
|
<0.01 |
|
No |
48 |
75 |
|
55 |
95 |
|
|
Yes |
52 |
25 |
|
45 |
5 |
|
|
Graft type |
|
|
0.84 |
|
|
<0.01 |
|
Bone marrow |
4 |
4 |
|
4 |
12 |
|
|
Peripheral blood |
96 |
96 |
|
96 |
88 |
|
|
Pre-transplant ruxolitinib |
|
|
0.03 |
|
|
<0.01 |
|
No |
51 |
38 |
|
41 |
57 |
|
|
Yes |
49 |
61 |
|
59 |
43 |
|
|
Missing |
0 |
1 |
|
0 |
0 |
|
In the RIC setting, fludarabine/melphalan was associated with significantly poorer outcomes compared with fludarabine/busulfan (Figure 1), including the following:
- Significantly worse 2-year adjusted OS (54.4% vs 60.9%)
- Higher risk of early non-relapse mortality (17.4% vs 4.3%)
- Higher risk of Grade 2–4 (40% vs 35.3%) and Grade 3–4 (21.8% vs 12.1%) acute GvHD
- Worse rate of 30-day neutrophil engraftment (92.4% vs 95.1%)
- Lower 100-day platelet engraftment (73.9% vs 84.4%)
In the MAC setting, busulfan/cyclophosphamide was associated with significantly higher risk of Grade 2–4 and 3–4 acute GvHD and inferior GRFS compared with fludarabine/busulfan (Figure 1).
Disease-free survival and risk of relapse were not significantly different based on the conditioning regimen used in both settings (Figure 1).
Figure 1. Multivariable analysis of outcomes based on conditioning regimen used in A RIC and B MAC settings*
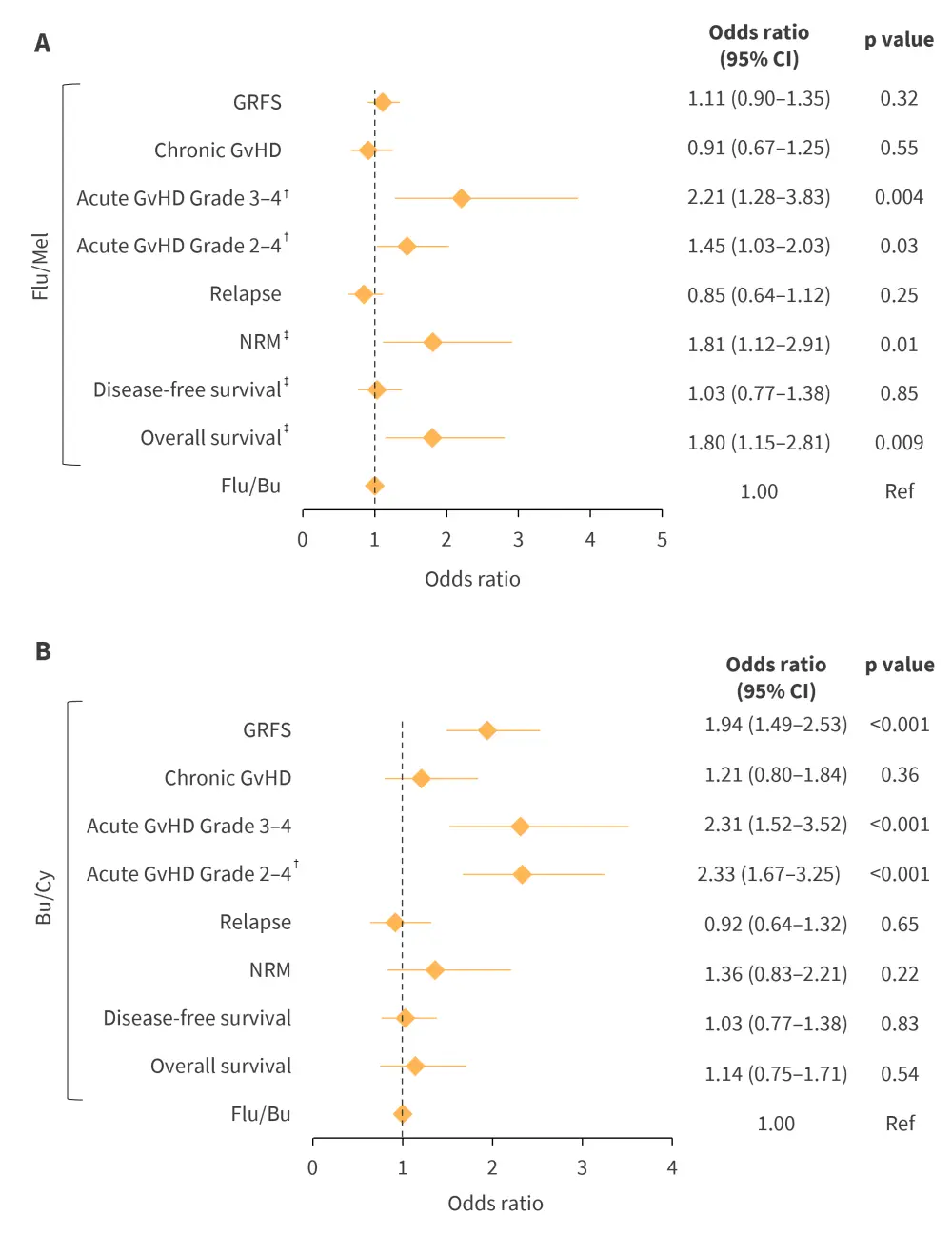
Bu, busulfan; CI, confidence interval; Cy, cyclophosphamide; Flu, fludarabine; GRFS, GvHD-free relapse-free survival; GvHD, graft-versus-host disease; Mel, melphalan; NRM, non-relapse mortality.
*Adapted from Murthy, et al.1
†≤2 months.
‡≤6 months.
Conclusion
The study suggested that fludarabine/busulfan conditioning in allo-HCT for MF was associated with superior OS, lower early non-relapse mortality and lower acute GvHD with RIC, and lower acute GvHD and superior GRFS with MAC. The results provide directions for tailoring the conditioning strategies to improve allo-HCT outcomes in MF. Further studies are warranted to validate these results and identify the ideal conditioning regimen in MF.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content


