All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MPN Advocates Network.
The mpn Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mpn Hub cannot guarantee the accuracy of translated content. The mpn and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The MPN Hub is an independent medical education platform, sponsored by AOP Health, GSK, Sumitomo Pharma, and supported through educational grants from Bristol Myers Squibb and Incyte. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MPN content recommended for you
Cumulative thrombotic risk between CALR1, CALR2 and JAK2V617F mutations in ET
Do you know... Patients with calreticulin (CALR) and Janus kinase 2 (JAK2) mutations have been shown to have different risks of developing thrombosis. Which of the following statements is true about mutation profile and thrombotic risk?
Thrombosis is one of the main complications experienced by patients diagnosed with essential thrombocythemia (ET) and confers significant morbidity and mortality.1 While it is well known that the presence of the Janus kinase 2 (JAK2)V617F mutation is an important risk factor for thrombosis, there is increasing evidence to suggest that other mutations, especially those involving calreticulin (CALR), may also increase thrombotic risk.1
As JAK2V617F and CALR mutations represent two distinct subtypes of ET, Neupane et al.1 performed a systematic review and meta-analysis in American Journal of Hematology, comparing the cumulative thrombotic risk between CALR1-, CALR2-, and JAK2V617F-mutated ET. Here, we summarize the key results.
For more information on the risk of thromboembolic complications in myeloproliferative neoplasms (MPN), check out this article and discussion from the MPN Hub Steering Committee published on the MPN Hub.
Study design
- Relevant peer-reviewed studies were searched across PubMed, Google Scholar, MEDLINE OVID, Cochrane Library, and Cumulative Index to Nursing and Allied Health Literature database
- Study publish date was set as from database inception to January 2023
- A total of 15 studies were selected for meta-analysis
- Most were retrospective in design
- 10 of the 15 studies were deemed to have a low bias risk, the rest had a moderate risk of bias
Results
- A total of 4,894 patients were analyzed:
- 795 patients had a CALR1 mutation;
- 561 patients had a CALR2 mutation; and
- 3,538 patients had a JAK2 mutation.
- The pooled odds ratios for thrombotic risk across the 15 studies are shown in Figure 1
Figure 1. Pooled odds ratios for thrombotic risk across all selected studies*
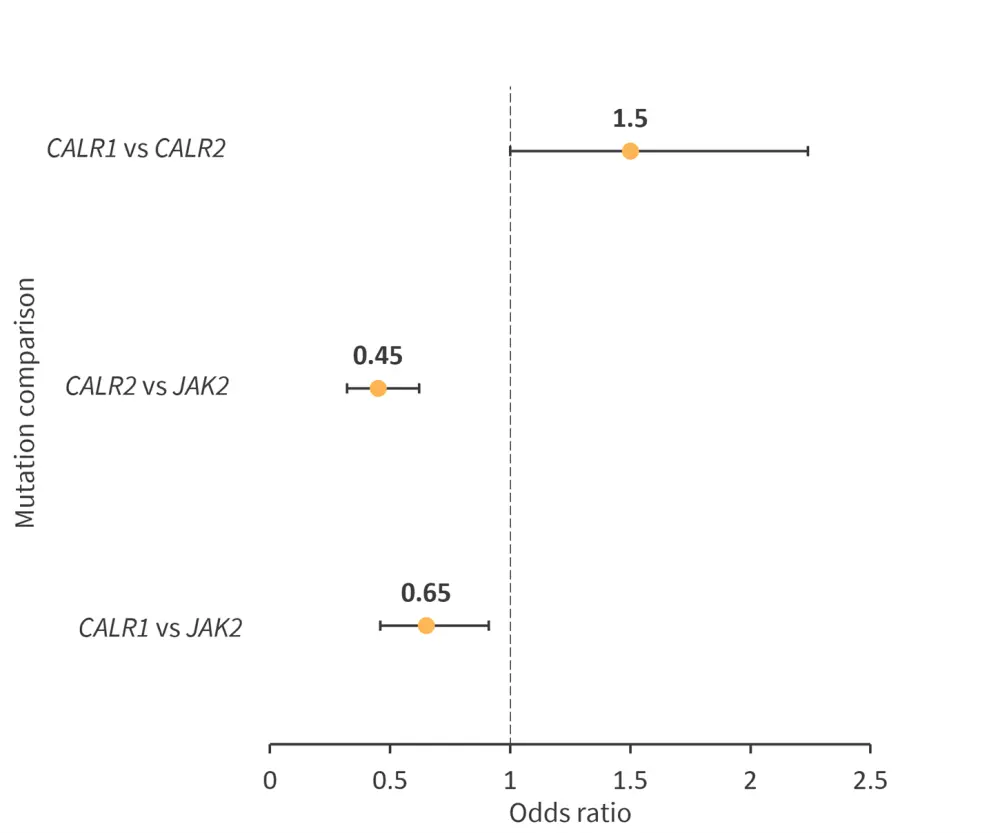
*Adapted from Neupane, et al.1
After sensitivity analysis and the removal of studies with medium and high bias risk, the pooled odds ratios of thrombotic risk across the remaining eight studies are shown in Figure 2.
Figure 2. Pooled odds ratios of thrombotic risk across eight studies post sensitivity analysis*
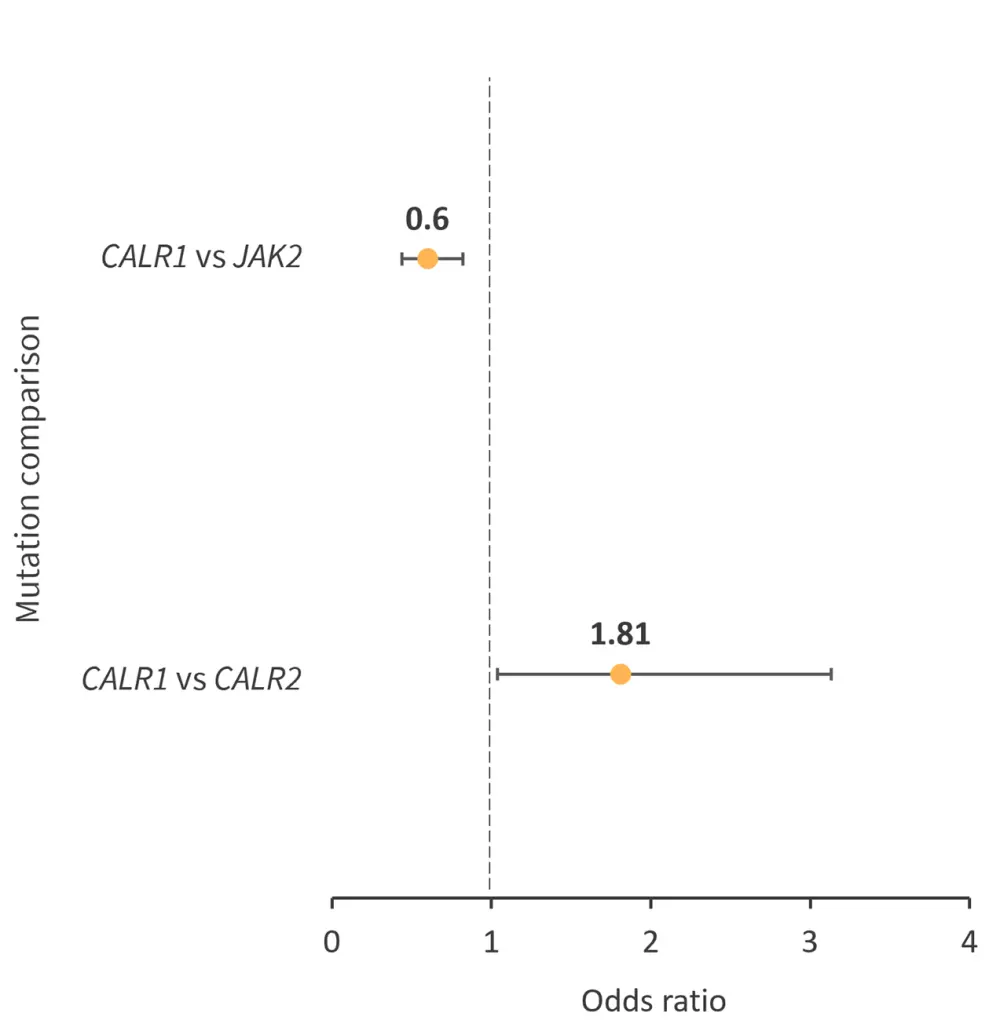
*Adapted from Neupane, et al.1
Subgroup analysis of the site of thrombosis did not reveal any statistically significant results; however, there was lower venous thrombotic risk in patients with a CALR2 mutation vs a JAK2 mutation.
Conclusion
Results from this meta-analysis show that patients with either a CALR1 or CALR2 mutation have a lower thrombotic risk compared with patients with a JAK2 mutation and patients with a CALR1 mutation have a higher risk of thrombosis vs patients with a CALR2 mutation. The pathophysiology underlying this difference remains unknown; however, it has been suggested that CALR2 reduces activation of the thrombopoietin receptor and adenosine diphosphate-induced platelet activation due to its lower net positive charge.
Limitations of this analysis include variations in population sizes, study designs, and follow-up periods. While further investigation is needed, the analysis highlights the potential and need for individual management strategies based on specific mutational profiles.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

