All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MPN Advocates Network.
The mpn Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mpn Hub cannot guarantee the accuracy of translated content. The mpn and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The MPN Hub is an independent medical education platform, sponsored by AOP Health, GSK, Sumitomo Pharma, and supported through educational grants from Bristol Myers Squibb and Incyte. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MPN content recommended for you
ZGJAK002 trial: Efficacy and safety of jaktinib in patients with MF
Jaktinib, a Janus kinase, and activin A receptor type I inhibitor, is a deuterated form of momelotinib and has shown promising results for treating patients with myelofibrosis (MF), specifically in spleen volume reduction and symptom relief.
Here, we summarize a long-term follow-up of the ZGJAK002 trial (NCT03886415) published by Zhang et al.1 in American Journal of Hematology assessing the safety and efficacy of jaktinib in Chinese patients with intermediate to high-risk MF.
Study design1
- Phase II, open-label dose comparison trial 30.7 months after trial initiation
- Patients (N = 118) were assigned 100 mg jaktinib twice daily (BID, n = 66) or 200 mg jaktinib once daily (QD, n = 52)
- The primary endpoint was the proportion of patients with ≥35% decrease in spleen volume (SVR35) at Week 24.
- Secondary endpoints included total symptom score improvement by ≥50% (TSS50), improvement in anemia, and safety profile.
Key findings1
- More patients achieved SVR35 with 100 mg BID vs 200 mg QD (Figure 1)
- The proportion of patients achieving spleen volume reductions increased over time, indicating durable responses
- TSS50 improvements and hemoglobin levels were sustained in both groups from Week 48 to Week 120 in long-term follow-up results (Table 1).
- No further safety signals were identified in either cohort, common Grade ≥3 adverse events outlined in Table 1.
Table 1. Key long-term efficacy and safety data for jaktinib 100 mg BID and 200 mg QD regimens*
- Median overall survival was not met by either cohort, with 36-month survival rates of 78.0% vs 73.6%, respectively
- Deaths were reported in 18.2% and 25%, respectively
Figure 1. SVR35 in patients with intermediate to high-risk MF treated with 100 mg BID or 200 mg QD jaktinib*
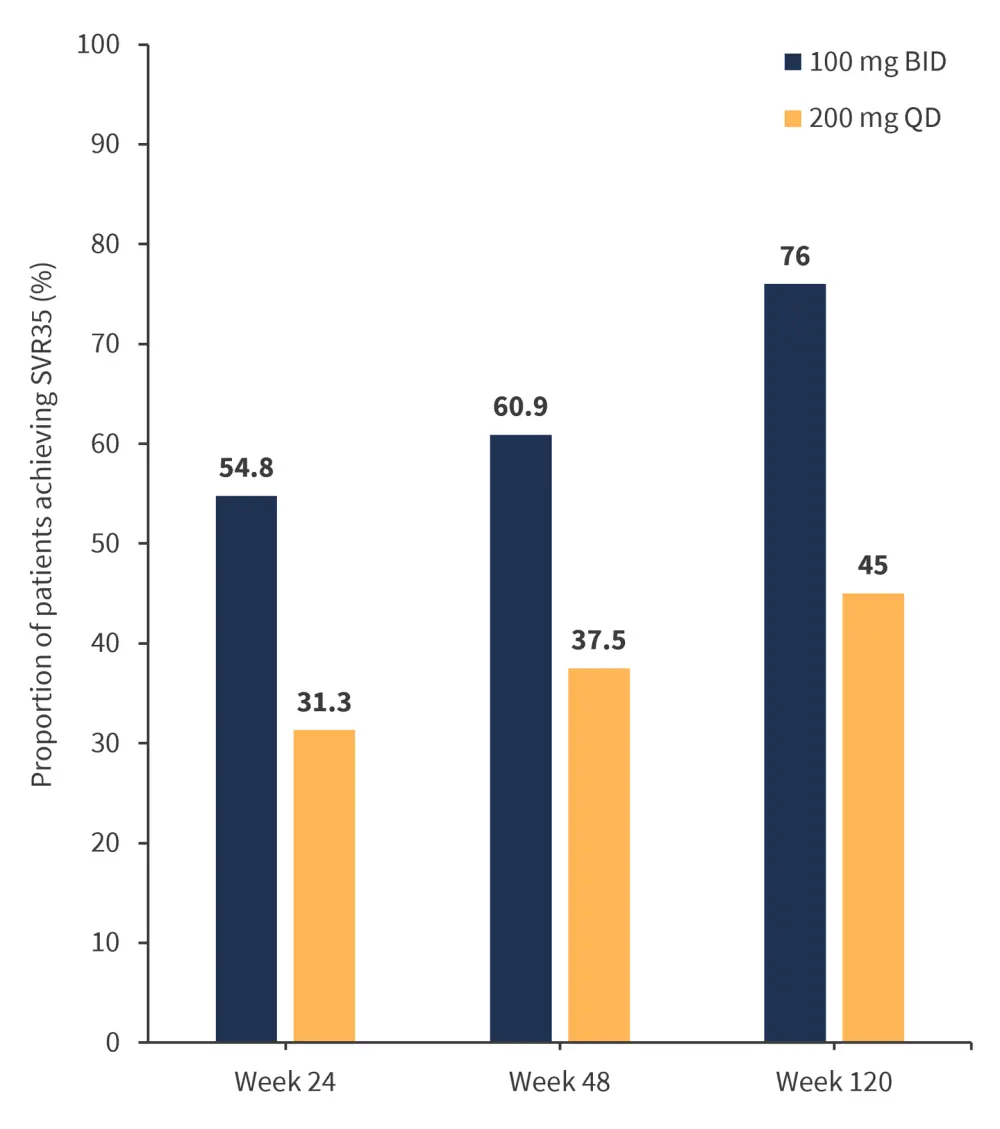
BID, twice daily; MF, myelofibrosis; QD, once daily; SVR35, spleen volume reduction ≥35%.
*Adapted from Zhang, et al.1
|
Key learnings |
|---|
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

