All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MPN Advocates Network.
The mpn Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mpn Hub cannot guarantee the accuracy of translated content. The mpn and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The MPN Hub is an independent medical education platform, sponsored by AOP Health, GSK, Sumitomo Pharma, and supported through educational grants from Bristol Myers Squibb and Incyte. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MPN content recommended for you
Pregnancy and MPN
Do you know... Pregnant patients with MPN face an increased risk of bleeding. At what stage of the pregnancy is the risk of venous thromboembolism highest?
There is a distinct set of challenges for patients who become pregnant and have a diagnosis of myeloproliferative neoplasms (MPN), as previously discussed on the MPN Hub. These patients have an increased risk of thrombosis and hemorrhage, especially during delivery and postpartum, in addition to consequences for fetal growth, including placental insufficiency, stillbirth, and premature delivery.1 As a result, complex management strategies are required to ensure the best possible maternal and fetal outcomes. Best practice recommendations for managing pregnant patients with MPN have previously been reported on the MPN Hub. Here, we outline common risks, challenges, and further practice recommendations in the management of this patient population.
Risks and challenges1
- Pregnancy-induced hypercoagulability presents a specific set of challenges.
- The risk of venous thromboembolism is increased 4- to 6-fold in these patients.
- This risk is greatest postpartum due to increased platelet counts and hematocrit levels.
- The risk of overall pregnancy complications is highest during the first trimester.
- As previously covered by the MPN Hub, fetal and maternal complications include maternal thrombosis, hemorrhage, and placental dysfunction
- Treatment options should be discussed with the patient prior to conception, due to some forms of MPN therapy being teratogenic.
Treatment options2
- Aspirin is prescribed to reduce the risk of pre-eclampsia and fetal death.
- Studies have shown increased live birth rates with aspirin treatment.
- Conversely, treatment with aspirin must be carefully considered if the patient has acquired von Willebrand syndrome, as the condition presents a further increased risk of bleeding.
- Patient clinical parameters are tested early in pregnancy and during the third trimester.
- Low molecular weight heparin treatment is recommended as prophylaxis against prior thrombotic events.
- Heparin should only be administered when the risk of venous thromboembolism is >3%, due to net clinical benefit.
- Heparin should not be administered if the risk is <1%.
- Venesection reduces hematocrit levels to predefined ranges according to each trimester:
- 0.31–0.41% (first trimester)
- 0.30–0.38% (second trimester)
- 0.28–0.39% (third trimester)
- If cytoreduction is imperative, the only recommended treatment is pegylated interferon alfa-2a as there are no current reports of teratogenesis.
- All other cytoreductive therapies, including hydroxyurea and anagrelide, are unusable in pregnant patients due to teratogenic effects.
Practice recommendations2
- Management strategies used to mitigate risks to mother and fetus are defined according to the stage of pregnancy (Figure 1).
Figure 1. Management strategies according to pregnancy stage in patients with MPN*
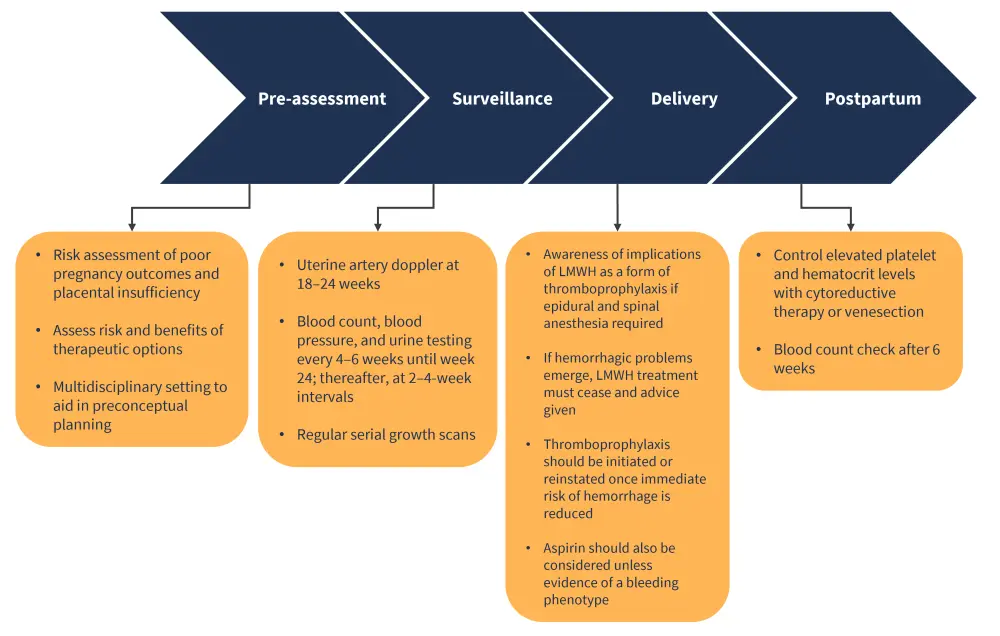
LMWH, low molecular weight heparin; MPN, myeloproliferative neoplasms.
*Adapted from Robinson and Harrison.2
Conclusion
Pregnant patients diagnosed with MPN require multidisciplinary management to ensure the strategies associated with each stage of pregnancy are implemented and optimized. While maternal and fetal outcomes are improving with current therapeutic options and risk-mitigating recommendations, further advancement and refinement of management strategies is warranted.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

