All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MPN Advocates Network.
The mpn Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mpn Hub cannot guarantee the accuracy of translated content. The mpn and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The MPN Hub is an independent medical education platform, sponsored by AOP Health, GSK, Sumitomo Pharma, and supported through educational grants from Bristol Myers Squibb and Incyte. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MPN content recommended for you
Rates of childbirth amongst women with myeloproliferative neoplasms
Pregnancies in patients with myeloproliferative neoplasms (MPN) are often associated with poorer outcomes, including an increased risk of pre-eclampsia, as well as maternal and fetal morbidity. However, there are limited data on childbearing and birthrates amongst patients with MPN compared with the general population.1
Here, we summarize a retrospective analysis by Landtblom et al.1 published in Leukemia on the childbirth rates in women with MPN.
Study design1
- Women with an MPN diagnosis, aged between 15 and 44 years, were selected from healthcare registers in Sweden.
- Patients were age-matched in a ratio of 1:4 with controls from the general population.
- The main outcome was time to first live childbirth post-MPN diagnosis.
- Subgroup analyses were performed by age and MPN subtype.
- Secondary outcomes were miscarriage rate, and stillbirth pre- and post-MPN diagnosis.
Key findings1
- A total of 1,141 patients with MPN and 4,564 control participants were included in this study.
- A 22% decreased childbirth rate was observed amongst the patients with MPN, compared with the control cohort (Figure 1).
- Essential thrombocythemia was the only subtype with similar childbirth rates to the control group.
- Childbirth rates were significantly reduced in all other MPN subtypes.
- Women aged 15–25 years were observed to have significantly reduced birthrates compared with the control group.
- No significant differences in birthrates were observed in any other age category.
- At the time of diagnosis, 61% of women with MPN had given birth to at least one child, compared with 67.3% in the age-matched controls (p < 0.001).
- With mean follow-up of 5 years, the risk of miscarriage was not significantly increased amongst patients with MPN compared with the control group; hazard ratio 1.25 (95% confidence interval [CI], 0.89–1.76).
- However, women with MPN were more likely to have experienced a previous stillbirth, with fewer children in total.
Figure 1. Hazard ratio of live births per MPN subtype and age at diagnosis*
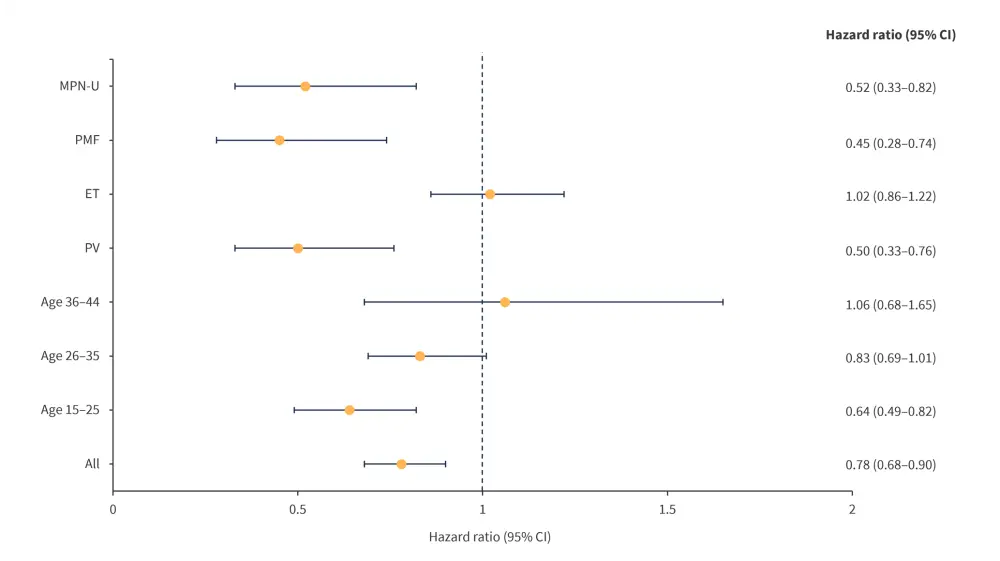
CI, confidence interval; ET, essential thrombocythemia; MPN-U, myeloproliferative neoplasms-unclassified; PMF, primary myelofibrosis; PV, polycythemia vera.
*Data from Landtblom, et al.1
|
Key learnings |
|---|
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content




