All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MPN Advocates Network.
The mpn Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mpn Hub cannot guarantee the accuracy of translated content. The mpn and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The MPN Hub is an independent medical education platform, sponsored by AOP Health, GSK, Sumitomo Pharma, and supported through educational grants from Bristol Myers Squibb and Incyte. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MPN content recommended for you
Parsaclisib in patients with MF and suboptimal ruxolitinib response
Intermediate- or high-risk myelofibrosis (MF) can be treated with ruxolitinib to reduce spleen size, manage symptoms, and increase survival.1 However, many patients have a suboptimal response to ruxolitinib or relapse over time. Therefore, treatments for post-ruxolitinib failure are currently under investigation.
Here, we summarize a phase II study by Yacoub et al.1 published in Blood Advances which investigates the addition of parsaclisib, a phosphoinositide 3-kinase inhibitor, for patients with MF who responded suboptimally to initial ruxolitinib treatment.
Study design1
- This study consisted of four parts:
- Eligible patients had received ruxolitinib ≥6 months at a dose of 5–25 mg twice daily for ≥8 weeks prior to the study start, with suboptimal response.
- The primary endpoints included:
- Part one: Determining a well-tolerated dose of parsaclisib in combination with ruxolitinib according to MF Symptom Assessment Form Scores (MFSAF).
- Part two to four: Absolute change and percentage change in spleen volume from baseline to Week 12.
- After the maximum and minimum doses had been investigated, patients were regrouped and randomized to either daily or daily to weekly parsaclisib dosing schedules (Figure 1).
Figure 1. Study design*
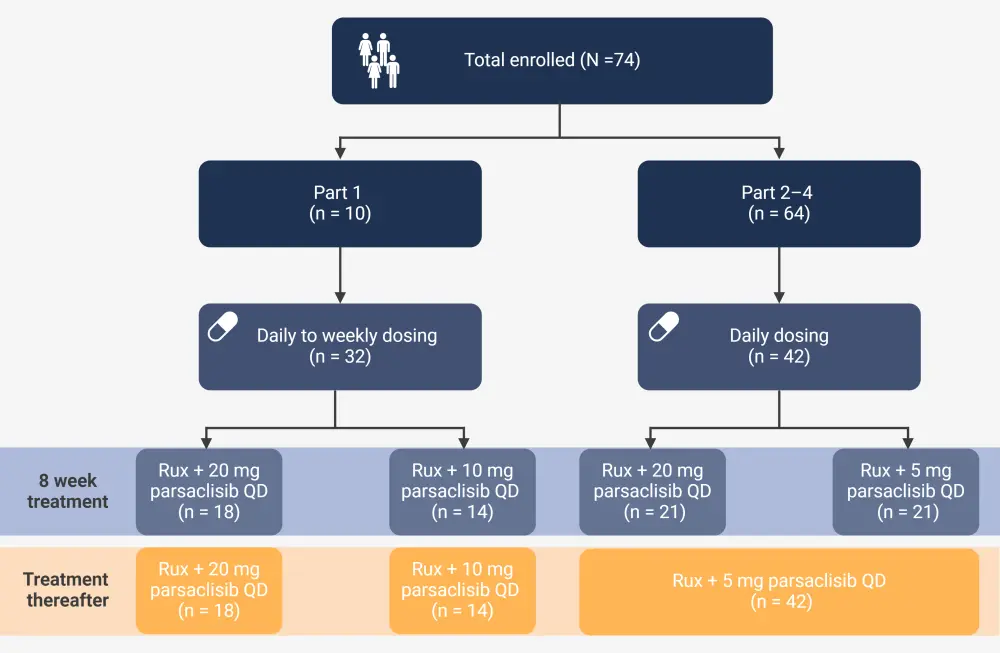
QD, once daily; QW, once weekly; Rux, ruxolitinib.
*Adapted from Yacoub, et al.1 Created with BioRender.com.
Key findings1
- Overall, 74 patients were enrolled across all parts of the study.
- Baseline characteristics were similar between groups, with a median age of 68 years and 47% male.
- In part one:
- The maximum tolerated dose of parsaclisib was 20 mg daily.
- No dose-limiting toxicities were reported.
- 96% of patients experienced ≥1 treatment-emergent adverse event and nausea was most reported (23%).
- In parts two to four:
- 88% of patients were evaluable for the primary endpoint of absolute change.
- Percentage change in spleen volume from baseline to Week 12, with the remaining patients not evaluable due to discontinuation.
- Among those who met the primary endpoint, the median percentage change of spleen volume from baseline to Week 12 was −11% (Figure 2).
- The median percentage change was greatest in patients receiving daily doses of parsaclisib compared with weekly.
Figure 2. Median percentage change of spleen volume from baseline, Week 12, and Week 24 in patients treated daily and weekly with parsaclisib after ruxolitinib treatment*
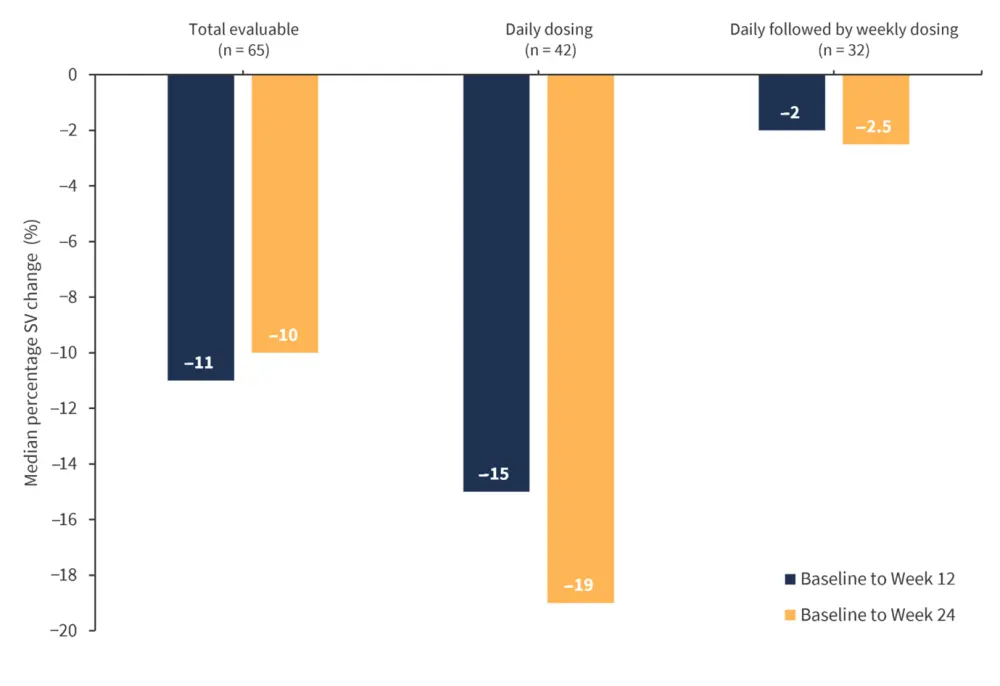
SV, spleen volume.
*Adapted from Yacoub, et al.1
- In a spleen volume reduction analysis from baseline to Week 12, 46% of patients achieved spleen volume reductions ≥10%;
- Patients who received daily doses of parsaclisib reported higher spleen volume reductions ≥10% than those who received daily-to-weekly dosing (59.5% vs 28%).
- Median percentage change in MFSAF from baseline to Week 12 was −20.5%;
|
Key learnings |
|---|
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content


