All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MPN Advocates Network.
The mpn Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mpn Hub cannot guarantee the accuracy of translated content. The mpn and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The MPN Hub is an independent medical education platform, sponsored by AOP Health, GSK, Sumitomo Pharma, and supported through educational grants from Bristol Myers Squibb and Incyte. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MPN content recommended for you
Diagnosis and treatment of pediatric patients with MPN
During the 2023 Global MPN Scientific Foundation (GMPNSF) Virtual Symposium entitled ‘Shining the light on pediatric, young adult, and pregnant patients living with MPNs’ held March 23–24, 2023, Kucine, Ianotto, and Randi discussed the special considerations in treating pediatric patients with myeloproliferative neoplasms (MPN).
The MPN Hub has previously reported on disease characteristics and outcomes in pediatric patients with MPN, highlighting the unique clinical presentations and outcomes in these patients compared with older adult patients. Here, we summarize the key considerations in diagnosing and treating pediatric patients with MPN.
Pediatric vs adult patients with MPN1,2
- MPN are very rare in children compared with adults.
- Diagnostic criteria, risk classification, and treatment guidelines in polycythemia vera (PV) and essential thrombocythemia (ET) focus mainly on adult patients.
- Patients need MPN-specific and age-specific treatment approaches, with different approaches in children vs adults and in ET vs PV.
- Diagnosis in children is particularly important due to the increased risk of reactive thrombosis.
Diagnostic considerations in pediatric patients1,2
- Differentiating between ET and other potential causes of symptoms must be carefully considered
- Diagnosing ET is simplified in the presence of JAK2 or CALR mutations
- Diagnosis is more challenging in patients with triple-negative mutations (absence of driver mutations in JAK2, MPL, and CALR), which is more common in pediatric patients than in adult patients
- It is important to differentiate between triple-negative ET and other potential causes of thrombosis
- Consideration of the bone marrow is important to ascertain whether the histology profile is consistent with MPN
- Diagnosis must be carefully evaluated and not rushed
- Monitoring over time is essential to identifying a clearer patient profile
- Subtle symptoms may indicate platelet reactivity
A suggested diagnostic work-up for a child being evaluated for MPN is outlined in Figure 1.
Figure 1. Suggested diagnostic work-up for a child being evaluated for MPN*
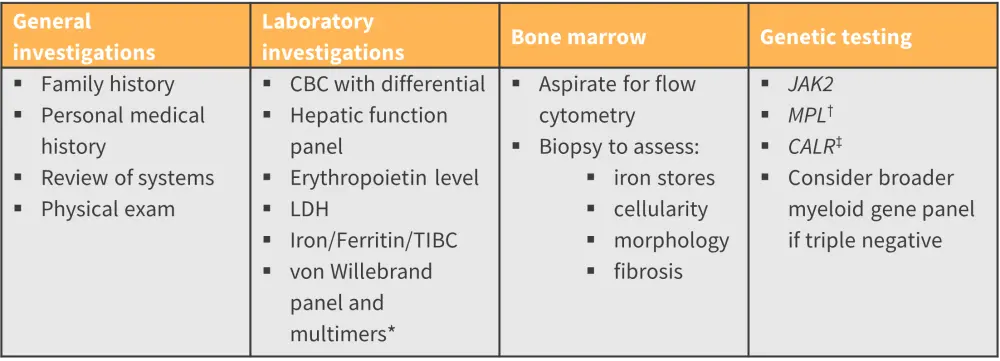
CBC, complete blood count; LDH, lactate dehydrogenase; MPN, myeloproliferative neoplasm; PMF, primary myelofibrosis; TIBC, total iron binding capacity.
*Adapted from Kucine, et al.2
†Acquired von Willebrand’s disease generally occurs with extreme thrombocytosis, generally this test is performed in patients with platelet counts >1000 × 109/L or with bleeding symptoms.
‡If JAK2 mutation is identified, testing for CALR and MPL mutations in ET, PMF, or pre-PMF patients is not indicated.
Treatment considerations in pediatric patients1,2
It is particularly important to consider why a child diagnosed with MPN might need treatment.1 The impacts of long term cytoreductive medications, abnormal blood counts on vasculature, increased cancer risk, cardiovascular risk, and fertility and pregnancy complications must be taken into account.2
- Platelet count does not directly correlate with thrombotic risk.
- A high platelet count does not necessarily drive treatment, especially in patients with no history of thrombosis.
- In adults, a platelet count of >1.5 × 106 generally indicates treatment; however, this is not necessarily the case for children.
- Children referred to a specialist may already have been prescribed a cytoreductive treatment, such as hydroxyurea, by their primary physician.
- In these cases, it is important to ascertain the rationale for treatment
- If the patient presented with a severe blood clot, the treatment is probably appropriate
Treatment options in pediatric patients1,2
While consensus guidelines have been published for the management of MPN in adults, literature on the treatment of pediatric patients is limited, with no data available indicating that the same risk stratification and scoring systems are applicable to both adults and children. From the available literature, the consensus is that fully asymptomatic children with MPN should not receive cytoreductive treatments, whilst children who have experienced thrombosis or severe hemorrhage should receive cytoreductive treatment.
No cytoreductive agents are approved for use in children with MPN; however, off-label use of the following are reported in clinical practice.1,2
- hydroxyurea
- interferon-α (IFN); pegylated interferon may offer improved tolerability
- anagrelide
- ruxolitinib; which is used rarely
Each treatment presents specific risks and benefits; these should be discussed with the child’s family before a treatment plan is agreed.
Conclusion1,2
The symposium offered a thorough and insightful discussion of special considerations in the diagnosis and treatment of pediatric patients with MPN. The speakers highlighted that available data are based primarily on experience in older patients and that it is paramount to adopt a flexible, adaptive approach in the pediatric setting. Whilst a high platelet count generally indicates treatment in adults, this is not necessarily the case in children. The risk/benefit profiles of cytoreductive treatments are very different between adults and children, these must be assessed carefully in the context of the full clinical picture; ensuring that children with MPN receive an appropriate diagnosis and treatment plan.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content




