All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the MPN Advocates Network.
The mpn Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mpn Hub cannot guarantee the accuracy of translated content. The mpn and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The MPN Hub is an independent medical education platform, sponsored by AOP Health, GSK, Sumitomo Pharma, and supported through educational grants from Bristol Myers Squibb and Incyte. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View MPN content recommended for you
Symposium | The treatment landscape for patients with myelofibrosis and anemia
Featured:
Do you know... Which of the following is true of new/worsening anemia in patients with myelofibrosis?
During the European School of Haematalogy (ESH) 4th How to Diagnose and Treat CML/MPN conference, the MPN Hub held a symposium on March 9, 2025, titled Anemia in myelofibrosis: Sequencing therapies to optimize patient outcomes. Here, we share a presentation by Francesco Passamonti, Università degli Studi di Milano, Milan, IT, discussing the treatment landscape for patients with myelofibrosis and anemia.
The treatment landscape for patients with myelofibrosis and anemia
The treatment landscape for patients with myelofibrosis and anemia
Firstly, Passamonti provided an overview of current treatment strategies for patients with myelofibrosis (MF)-related anemia, including red blood cell transfusion, erythropoiesis-stimulating agents, androgens, splenectomy, immunomodulatory drug agents, and Janus kinase inhibitors (JAKis).1 He then discussed key efficacy and safety data from phase III trials of ruxolitinib, fedratinib, pacritinib, and momelotinib, with a focus on anemia.
Ruxolitinib
The phase III COMFORT-I (NCT00952289) and COMFORT-II (NCT00952289) trials demonstrated the spleen response benefit of ruxolitinib vs placebo and best available therapy (BAT), respectively (Figure 1).2,3
Figure 1. SVR35 response rates in the COMFORT-I and COMFORT-II trials*
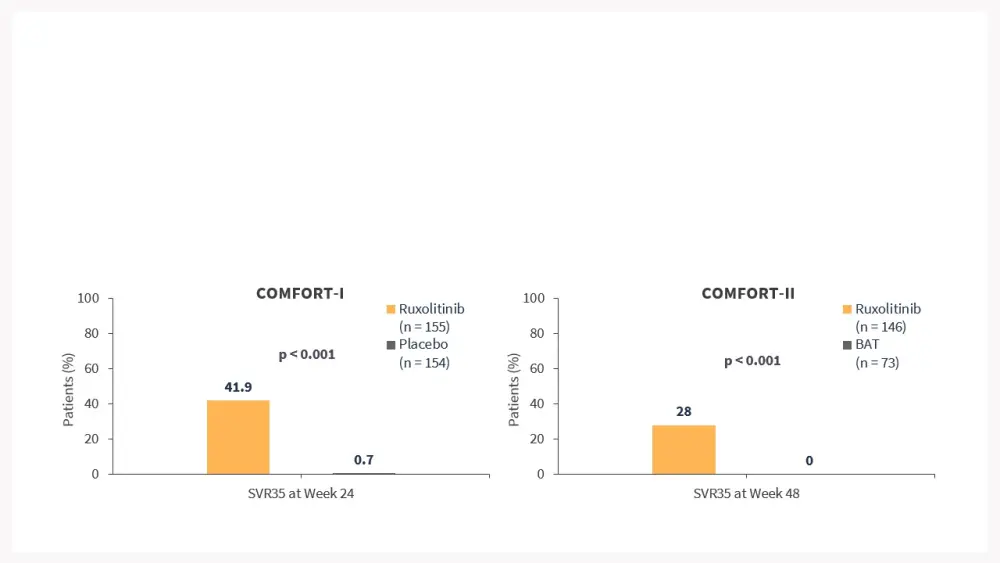
The majority of patients treated with ruxolitinib in the COMFORT-I (96%) and COMFORT-II (97%) trials were anemic, and almost 50% of patients in both trials became transfusion dependent.2–4
The efficacy of ruxolitinib is dose-dependent, as shown in the phase IIIb JUMP (NCT01493414) trial, which included patients with low platelet (PLT) counts (50 to <100 × 109/L); lower ≥50% spleen volume reduction (SVR) rates were observed in patients with low PLT counts who received lower doses of ruxolitnib.5
Results from the JUMP trial and a real-world study of adult patients with MF who were treated with ruxolitinib in the US Flatiron database demonstrated that new or worsening anemia was associated with worse overall survival in patients who were nonanemic at baseline.6,7
The response to ruxolitinib after 6 months (RR6) model includes anemia as a risk factor for worse survival among patients treated with ruxolitinib.8
Fedratinib
Results from the phase III JAKARTA (NCT01437787),9,10JAKARTA-2 (NCT01523171),9,11FREEDOM (NCT03755518),12 and FREEDOM-2 (NCT03952039)13 trials showed that fedratinib has similar efficacy to ruxolitinib in terms of spleen response; however, anemia was a common adverse event.
Pacritinib
Results from the phase III PERSIST-1 (NCT01773187) and PERSIST-2 (NCT02055781) trials demonstrated the benefit of pacritinib vs BAT in patients with MF, with no exclusions for baseline anemia or thrombocytopenia in PERSIST-1, and patients with PLT count ≤100 × 109/L in PERSIST-2 (Figure 2).14,15
A subanalysis from PERSIST-2 showed that patients treated with pacritinib had improved transfusion independence (TI) rates vs BAT when assessed using the Gale criteria (37% vs 7%; p = 0.001) and the SIMPLIFY criteria (24% vs 4.5%; p = 0.013).16
Figure 2. Response rates in the PERSIST-1 and PERSIST-2 trials*
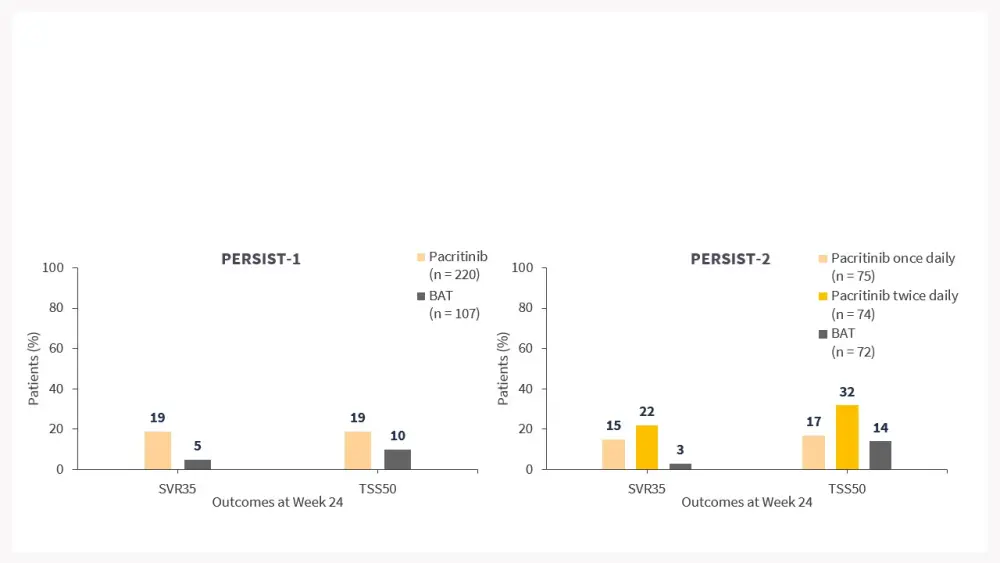
A pooled analysis from the PERSIST-1 and PERSIST-2 trials found that pacritinib improved SVR35 (23% vs 2%; p = 0.0007) and 50% reduction in total symptom score (TSS; 25% vs 8%; p = 0.0441) vs BAT in patients with PLT count <50 × 109/L (n = 189).17
Momelotinib
In the SIMPLIFY-1 (NCT01969838) trial, momelotinib demonstrated similar SVR35 response rates to ruxolitinib (26.5% vs 29.0%; noninferiority p = 0.011), and improved TI rates (66.5% vs 49.3%; p <0.001) in JAKi-naïve patients (Figure 3).18
Mean hemoglobin levels increased in patients who crossed over from ruxolitinib to momelotinib.19
Figure 3. Response rates in the SIMPLIFY-1 trial*
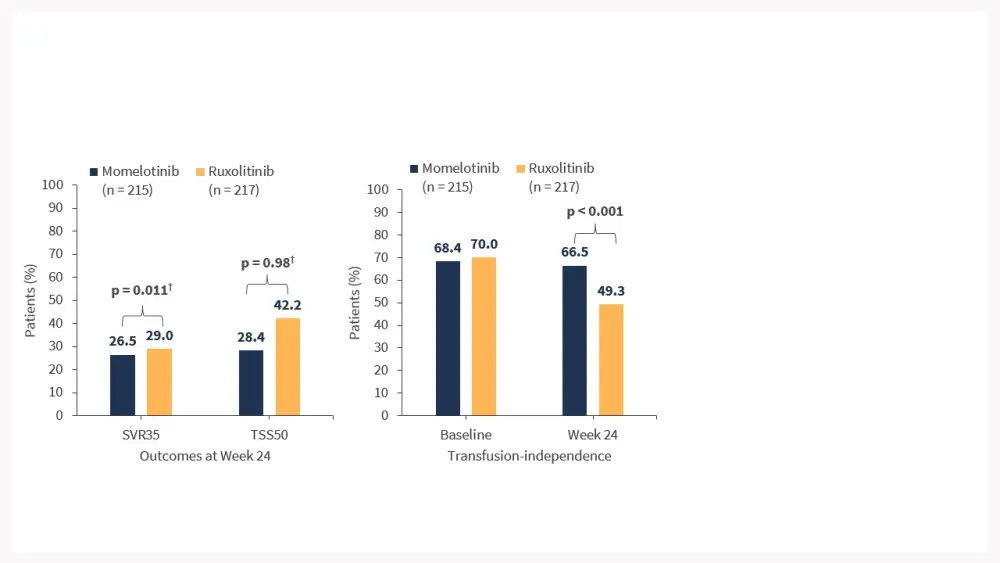
Results from SIMPLIFY-2 showed similar rates of SVR35 response between momelotinib and BAT (7% vs 6%; p = 0.90), while momelotinib was associated with improved TSS50 (26% vs 6%; p = 0.0006) and TI rates (43% vs 21%; p = 0.0012) in JAKi-experienced patients.20
Patients who crossed over from BAT to momelotinib had increased mean hemoglobin levels.21
In the phase III MOMENTUM trial (NCT04173494) trial, the TSS50, TI, and SVR35 rates at Week 48 among patients treated with momelotinib were 45%, 57%, and 43%, respectively, and among patients who crossed over from the danazol to momelotinib, the response rates were 50%, 60%, and 13%, respectively.22
Conclusions
Passamonti concludes by highlighting the following:
Ruxolitinib and fedratinib can effectively improve splenomegaly; however, they may exacerbate anemia in patients with MF.
Results from the PERSIST trials suggest that pacritinib is effective in patients with MF and severe thrombocytopenia.
Data from the SIMPLIFY and MOMENTUM trials indicate that momelotinib can improve TI in patients with MF and anemia while also reducing splenomegaly.
A tailored approach may be necessary when choosing a JAKi for patients with MF, particularly if the patient presents with or develops anemia or severe thrombocytopenia.
This independent educational activity is supported by GSK. All content is developed independently by the faculty; the funder is allowed no influence on the content.
Your opinion matters
What do you consider to be the highest unmet need for patients with myelofibrosis?
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content


 Francesco Passamonti
Francesco Passamonti


